Article
Identifying and Managing Ankle Fractures in Older Patients
The incidence of ankle fractures in the older patient population is rising. These fractures are characterized as fragility fractures associated with osteoporosis, but propensity for falls, increased weight, and polypharmacy may be bigger risk factors than poor bone quality.
ABSTRACT: The incidence of ankle fractures in the older patient population is rising. These fractures are characterized as fragility fractures associated with osteoporosis, but propensity for falls, increased weight, and polypharmacy may be bigger risk factors than poor bone quality. Operative fixation is widely accepted as the proper treatment for younger patients, but the optimal treatment for older patients is less clear. The literature supports operative intervention for displaced ankle fractures in older patients. However, the presence of osteoporosis may increase the complexity of these cases, potentially requiring alteration of standard operative techniques. Orthopedic surgeons and primary care physicians need understanding of the risk factors associated with ankle fractures in older patients as well as appropriate evaluation and management strategies. (J Musculoskel Med. 2011;28:137-147)
Management of ankle fractures in older patients is a growing problem that affects the practices of both orthopedic surgeons and primary care physicians. Ankle fractures are common in older patients, and both their incidence and severity have increased significantly in this patient population during the past 30 years. In the United States, ankle fractures have been reported to occur in as many as 8.3 persons per 1000 Medicare recipients.1 Kannus and associates2 reported that the number of ankle fractures in Finnish patients older than 70 years increased 3-fold between 1970 and 2000. They also showed an increase in the more severe Lauge-Hansen supination-eversion stage 4 ankle fracture, compared with more stable ankle fracture patterns.
To achieve successful treatment outcomes, physicians need a clear understanding of the risk factors associated with ankle fractures in older patients as well as appropriate evaluation and management strategies. Ankle fractures in older patients typically result from low-energy injuries that involve a twisting mechanism, possibly reflecting the relative strength of the ankle ligaments and osteopenic bone. Recent studies have shown that propensity for falls, increased weight, and polypharmacy may play a larger role than osteoporosis does in the occurrence of ankle fractures in older patients; these findings challenge the categorization of ankle injuries in older persons as fragility fractures.
There is no consensus about what constitutes optimal management of ankle fractures in this potentially complex patient population. Most orthopedic surgeons agree that operative intervention is appropriate for younger patients with ankle fracture. However, treatment of injured older patients is controversial.3 Conservative treatment has been recommended for older patients because of poor outcomes after surgery in patients with osteoporosis and medical comorbidities, such as diabetes mellitus (DM) and peripheral vascular disease.4-7
In this article, we review the risk factors for ankle fracture in older patients, appropriate patient evaluation, and initial management strategies. We also describe data supporting operative or nonoperative management to help primary care physicians determine whether to treat or refer the older patient with ankle fracture.
DIAGNOSISRisk factors
Most clinical studies that evaluate ankle fractures in older patients have identified female sex, DM, and obesity as the main predictors of injury.8 Some investigators have categorized ankle fractures as osteoporotic fragility fractures on the basis of the high incidence of ankle fractures in postmenopausal women.9,10 However, observational studies have shown that the incidence of ankle fracture in older women increases until age 65 and then either plateaus or declines; this finding contradicts the notion that bone quality and fracture risk are associated.8,11-15 The increase in the number of ankle fractures seen in the older patient population may be a function of active older adults increasing in number rather than the presence of osteoporosis.

Clinical studies have examined the relationship of bone mineral density (BMD) to ankle fracture incidence in older patients and identified risk factors for these injuries (Table 1). In an evaluation of 9704 women older than 65 years, Seeley and colleagues15 found that after adjusting for age, the risk of ankle fracture was increased in women who had a history of falls in the previous year, were heavier, used their arms to rise from a chair, and either engaged in strenuous physical activity or rarely left their homes. The authors found no significant relationship between peripheral BMD and the incidence of ankle fracture in this patient cohort. They concluded that the risk factors for ankle fracture in older women are different from those associated with typical osteoporotic fragility fractures of the hip, distal radius, or proximal humerus.
In the Kuopio Osteoporosis Risk Factor and Prevention (OSTPRE) study of 11,798 older Finnish women, Valtola and coworkers16 found 4 independent predictors for ankle fracture in this patient population: overweight status, previous fracture history, polypharmacy, and cigarette smoking. The investigators identified a dose-response relationship between smoking and ankle fracture risk: the hazard ratio increased from 1.73 for study participants who smoked less than 1 pack of cigarettes per day to 2.94 for those who smoked more than 1 pack. In the OSTPRE study, patients who were taking 3 or more prescription drugs were twice as likely to sustain an ankle fracture as those who were not taking any prescribed medication.
Greenfield and Eastell9 used dual-energy x-ray absorptiometry scanning and quantitative ultrasonography to compare 103 women aged 50 to 80 years who had ankle fractures with 375 controls of similar age. They found no significant difference in BMD in the patient cohorts, except for in the trochanteric region, where patients with ankle fracture had a higher BMD than the population-based group. However, the authors did find that the ankle fracture population had a significantly higher body mass index than the controls. They concluded that increased body weight may contribute to a fracture about the ankle by increasing the forces applied to the ankle during a fall.
Anatomy
The ankle is a hinge type of synovial joint located between the distal ends of the tibia and fibula (the malleoli) and the superior part of the talus. The distal end of the tibia (the plafond) and the medial and lateral malleoli form a mortise, which provides a constrained articulation with the dome of the talus. The tibial plafond is wider anteriorly than posteriorly and is concave in both the sagittal and coronal planes, creating intrinsic stability with weight bearing by allowing for congruency with the trapezoidal shape of the superior aspect of the talus.
Ankle stability during motion is provided by the interosseous ligament between the tibia and fibula, the joint capsule, and the medial and lateral ligament complexes. The lateral ligament complex (weaker than the medial ligament complex) is composed of the anterior and posterior talofibular ligaments (which stabilize against anterior and posterior talar subluxation, respectively) and the calcaneofibular ligament (which provides restraint against inversion forces).
The superficial portion of the medial ligament complex (deltoid ligament) has fibers that fan out from their attachment to the medial malleolus and attach distally to the navicular, calcaneus, and talus to form the tibionavicular ligament, tibiocalcaneal ligament, and superficial ligaments, respectively. The deep portion of the deltoid (the deep tibiotalar ligament) is an intra-articular structure that acts as the primary stabilizer against lateral talar displacement with weight bearing and ankle motion. The combination of congruent bony anatomy and ligamentous structures provides stability to the tibiotalar joint during plantar flexion, dorsiflexion, inversion, and eversion.
Patient presentation
and evaluation
Older patients with an ankle fracture typically present with pain, swelling, and deformity about the injured ankle and an inability to bear weight on the affected side. The patient usually reports having sustained a twisting injury in which the foot twisted relative to the rest of the lower extremity. Determining the direction of rotational force at the time of injury may help predict the fracture pattern; however, most patients cannot recall the exact nature of the event. The patient’s history also should include a detailed account of his or her medical history and use of associated medications.
Epidemiological studies have demonstrated that ankle fractures of each mechanistic subtype (supination–external rotation, supination-adduction, pronation-abduction, and pronation–external rotation) occur in older patients. Supination–external rotation fractures are the most common type (Figure). They occur in the following 4 stages:
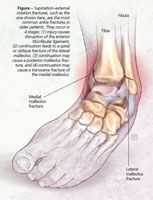
•Stage 1: Injury causes disruption of the anterior tibiofibular ligament with or without an avulsion fracture at its tibial or fibular insertions.
•Stage 2: Continuation leads to a spiral or oblique fracture of the lateral malleolus with a fracture line that runs from anteroinferior to posterosuperior.
•Stage 3: Continuation causes either a posterior malleolus fracture or a disruption of the posterior tibiofibular ligament.
•Stage 4: Continuation causes either a transverse fracture of the medial malleolus or a deltoid ligament rupture.
The significant increase reported in the most severe (stage 4) fracture type is important. Because these fractures are unstable, they will require operative intervention.
Physical examination
A complete physical examination helps physicians make the cor-rect diagnosis; the examination should include a careful neurovascular evaluation. Indicative of bony injury to the ankle are gross deformity, ecchymosis, swelling, point tenderness, and a palpable defect about the malleoli.
Assessment of ankle range of motion may not be possible in the acute stage of the injury if there is significant pain and swelling. The entire affected lower extremity should be palpated; particular attention should be paid to the proximal fibula and the base of the fifth metatarsal.
Palpation of the entire lower extremity is done primarily to rule out associated fractures. A fracture of the proximal fibula may occur with an ankle injury if a pronation–external rotation mechanism is present. The energy associated with this injury causes a medial malleolus fracture and may travel proximally along the syndesmosis (interosseous membrane), exiting through a proxi-mal fibular fracture. This injury, termed a Maisonneuve fracture, requires operative management.
The base of the fifth metatarsal is palpated to rule out fractures that often are associated with ankle injuries-Jones or pseudo-Jones fractures. Ankle dislocations and dislocations at these other sites usually are clinically obvious.
Appropriate radiographic evaluation of suspected ankle fractures includes anteroposterior, lateral, and mortise views of the affected side. These views typically enable the physician to clearly identify the fracture pattern, which dictates the approach to treatment. Medial-sided tenderness to palpation in the absence of a medial malleolar fracture warrants a stress view of the ankle so that a Lauge-Hansen supination-eversion stage 4 equivalent injury can be ruled out.
Ankle fractures and ankle sprains may involve similar patient histories, presentations, and examinations. A true determination of whether the injury is a fracture or sprain may be made with x-ray evaluation ordered according to the Ottawa Ankle Rules.
TREATMENTInitial management
For an isolated nondisplaced lateral malleolus fracture without evidence of syndesmotic ligament disruption, initial management should be nonoperative, including full weight bearing through the use of a cast brace or walking cast. Unstable fracture patterns with bimalleolar involvement and single malleolus fractures with associated talar displacement require reduction and splint immobilization; there should be no weight bearing on the affected side.
Further management:
operative versus nonoperative
Currently, consensus about the appropriate operative indications for ankle fracture in the older patient population is lacking because of a high rate of postoperative complications reported in early clinical studies. Several clinical investigations have evaluated the efficacy of surgical management versus conservative treatment; the results have been variable (Table 2).

In a prospective randomized trial of 84 patients older than 65 years who had displaced ankle fractures, Salai and associates6 found that at a mean follow-up of 37.5 months, patients treated nonoperatively had significantly higher clinical outcome scores than those treated operatively. Most frequently used and referenced is the American Orthopaedic Foot & Ankle Society (AOFAS) scoring system. Up to 40 points are assigned to the level of pain, 10 points to level of function, 5 points to maximum walking distance, 5 points to type of surface the patient can walk on, 8 points to gait (absence of abnormality), 8 points to sagittal motion, 6 points to hindfoot motion, 8 points to ankle-hindfoot stability, and 10 points to ankle alignment. The outcome score is total points out of a maximum of 100.
In addition, a high percentage of patients in the operative arm required re-operation for removal of hardware. As a result, the total cost of treatment per patient was almost 5 times higher than in patients treated nonoperatively.
Beauchamp and colleagues4 compared outcomes of operative and nonoperative management of 126 ankle fractures in patients older than 50 years. They found no significant difference in symptoms or ankle range of motion at a mean of 2 years of follow-up. However, surgical management led to an increased frequency of complications. Because of their findings, the authors of both studies concluded that conservative management is preferable in this patient population.
Other investigators have found that operative intervention leads to improved outcomes compared with nonoperative treatment. Makwana and colleagues17 conducted a prospective randomized trial of 47 patients older than 55 years who had displaced ankle fractures. They found significantly higher functional outcome scores, greater ankle range of motion, and less swelling in patients who were treated operatively than in those treated nonoperatively. In addition, patients who were treated with cast immobilization were less likely to have an anatomic reduction and more likely to lose their reduction during the treatment course.
Ali and coworkers18 conducted a retrospective review of 100 ankle fractures in patients older than 60 years. The rates of nonunion and malunion were significantly higher after conservative treatment, and patients who were treated operatively had a higher level of satisfaction than their nonoperative counterparts.
Retrospective reviews of the results after open reduction and internal fixation for ankle fractures in older patients showed high rates of fracture union and low rates of postoperative complications.3,7 In a study from our institution, Davidovitch and associates19 compared the functional outcome after surgical stabilization of ankle fractures in a patient population older than 60 years and a population younger than 60 years. They found that although functional recovery in older patients with ankle fracture occurs at a slower rate than in younger patients, a steady improvement was seen during the first postoperative year. Total AOFAS scores were similar in the 2 groups at 3, 6, and 12 months postoperatively. The authors concluded that operative fixation of unstable ankle fractures in older patients provides a reasonable postoperative functional result.
Treatment strategies
Although osteoporosis does not appear to be a significant risk factor for ankle fracture, it presents difficulties during operative management of ankle fractures in older patients. Because there is potential for poor screw fixation in osteoporotic bone, some authors recommend modifications of the standard surgical technique.20
Koval and colleagues21 reported on the use of 2 intramedullary Kirschner wires to augment lateral plate fixation of comminuted or osteopenic ankle fractures in 20 patients older than 50 years. Use of this technique resulted in a 100% rate of fracture union; about 90% of patients reported either no or mild postoperative pain. Biomechanical evaluation of this augmentation technique on cadaveric fibulae showed greater resistance to bending and torsional loading compared with fibula stabilization with a lateral plate alone.
Locked plating systems have been used to improve fixation in osteoporotic bone (the screws lock directly into the plate, creating a fixed angle construct). Locked plate designs offer better resistance against the torsional and bending forces associated with the toggling and pull out of conventional screws. In addition, locked plates do not need to be compressed onto bone; therefore, the local blood supply is preserved and the risk of primary loss of fracture reduction is limited.22 The ability of locked plating systems to improve fixation in poor-quality bone probably will increase their use in osteoporotic ankle fractures. However, this somewhat new technology has yet to be investigated adequately in this patient population.
Cement augmentation has been used to improve screw purchase in osteoporotic bone in hip and calcaneus fracture management; its utility can be applied to ankle fractures. After injection, the cement hardens, thus filling bony defects and improving the holding strength of inserted screws.23 Animal studies have shown that screw pullout strength and the overall load required for failure increase significantly with the use of calcium phosphate cement augmentation.24,25 By improving fixation strength and stability, cement augmentation may allow a patient a more rapid return to weight bearing and improve the overall outcome after operative ankle fracture repair.
Postoperative rehabilitation
Common postoperative rehabilitation protocols include starting range of motion exercises with a physical therapist shortly after surgery.20 Partial weight bearing (about 50 lb) typically is started at 8 weeks postoperatively; advancement is made as tolerated until full weight bearing is achieved, typically by 12 to 14 weeks. The possible addition of a postoperative boot for protection is subject to surgeon preference. A coordinated rehabilitation program provides older patients who have ankle fracture with the best opportunity for a quick return to function.
Postoperative complications
Orthopedic surgeons and primary care physicians must recognize that although postoperative complications in older patients with ankle fracture are somewhat infrequent, they can have a significant impact on treatment outcomes. The complications most frequently reported after surgical management of ankle fractures include wound-healing problems, infection, painful prominent hardware, and malunion.
The medical comorbidities that affect older patients with ankle fracture play an important role in both the incidence and type of postoperative complication. DM, a common medical problem in older patients, is a significant risk factor for complication after operative ankle fracture management. McCormack and Leith26 conducted a case-control study of 26 patients who had DM and ankle fracture matched for age, fracture type, and method of management. They reported a 31.6% incidence of major postoperative complications, including 2 cases of deep infection, 1 case of malunion, and 1 case of wound edge necrosis. Both patients in whom deep infection developed required amputation and subsequently died. In a review of postoperative complications after operative ankle fracture repair, Bibbo and coworkers27 reported that complications occurred in 46% of their patients with DM.
References:
References
1. Koval KJ, Lurie J, Zhou W, et al. Ankle fractures in the elderly: what you get depends on where you live and who you see. J Orthop Trauma. 2005;19:635-639.
2. Kannus P, Palvanen M, Niemi S, et al. Increasing number and incidence of low-trauma ankle fractures in elderly people: Finnish statistics during 1970-2000 and projections for the future. Bone. 2002;31:430-433.
3. Pagliaro AJ, Michelson JD, Mizel MS. Results of operative fixation of unstable ankle fractures in geriatric patients. Foot Ankle Int. 2001;22:399-402.
4. Beauchamp CG, Clay NR, Thexton PW. Displaced ankle fractures in patients over 50 years of age. J Bone Joint Surg. 1983;65B:329-332.
5. Litchfield JC. The treatment of unstable fractures of the ankle in the elderly. Injury. 1987;18:128-132.
6. Salai M, Dudkiewicz I, Novikov I, et al. The epidemic of ankle fractures in the elderly-is surgical treatment warranted? Arch Orthop Trauma Surg. 2000;120:511-513.
7. Srinivasan CM, Moran CG. Internal fixation of ankle fractures in the very elderly. Injury. 2001;32:559-563.
8. Daly PJ, Fitzgerald RH Jr, Melton LJ, Ilstrup DM. Epidemiology of ankle fractures in Rochester, Minnesota. Acta Orthop Scand. 1987;58:539-544.
9. Greenfield DM, Eastell R. Risk factors for ankle fracture. Osteoporos Int. 2001;12:97-103.
10. Kröger H, Huopio J, Honkanen R, et al. Prediction of fracture risk using axial bone mineral density in a perimenopausal population: a prospective study. J Bone Miner Res. 1995;10:302-306.
11. Baron JA, Barrett J, Malenka D, et al. Racial differences in fracture risk. Epidemiology. 1994;5:42-47.
12. Bengnér U, Johnell O, Redlund-Johnell I. Epidemiology of ankle fracture 1950 and 1980: increasing incidence in elderly women. Acta Orthop Scand. 1986;57:35-37.
13. Nilsson BE. Age and sex incidence of ankle fractures. Acta Orthop Scand. 1969;40:122-129.
14. Riggs BL, Melton LJ 3rd. Clinical review 8: clinical heterogeneity of involutional osteoporosis: implications for preventive therapy. J Clin Endocrinol Metab. 1990;70:1229-1232.
15. Seeley DG, Kelsey J, Jergas M, Nevitt MC. Predictors of ankle and foot fractures in older women. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1996;11:1347-1355.
16. Valtola A, Honkanen R, Kröger H, et al. Lifestyle and other factors predict ankle fractures in perimenopausal women: a population-based prospective cohort study. Bone. 2002;30:238-242.
17. Makwana NK, Bhowal B, Harper WM, Hui AW. Conservative versus operative treatment for displaced ankle fractures in patients over 55 years of age: a prospective, randomised study. J Bone Joint Surg. 2001;83B:525-529.
18. Ali MS, McLaren CA, Rouholamin E, O’Connor BT. Ankle fractures in the elderly: nonoperative or operative treatment. J Orthop Trauma. 1987;1:275-280.
19. Davidovitch R, McLaurin TM, Tejwani NC, et al. Functional outcome after surgically treated ankle fractures: does age matter? Presented at: 73rd Annual Meeting of the American Academy of Orthopaedic Surgeons; March 22-26, 2006; Chicago.
20. Cole PA, Craft JA. Treatment of osteoporotic ankle fractures in the elderly: surgical strategies. Orthopedics. 2002;25:427-430.
21. Koval KJ, Petraco DM, Kummer FJ, Bharam S. A new technique for complex fibula fracture fixation in the elderly: a clinical and biomechanical evaluation. J Orthop Trauma. 1997;11:28-33.
22. Wagner M. General principles for the clinical use of the LCP. Injury. 2003;34(suppl 2):B31-B42.
23. Larsson S, Bauer TW. Use of injectable calcium phosphate cement for fracture fixation: a review. Clin Orthop Relat Res. 2002;395:23-32.
24. Hutchinson GS, Griffon DJ, Siegel AM, et al. Evaluation of an osteoconductive resorbable calcium phosphate cement and polymethylmethacrylate for augmentation of orthopedic screws in the pelvis of canine cadavers. Am J Vet Res. 2005;66:1954-1960.
25. Leung KS, Siu WS, Li SF, et al. An in vitro optimized injectable calcium phosphate cement for augmenting screw fixation in osteopenic goats. J Biomed Mater Res B Appl Biomater. 2006;78:153-160.
26. McCormack RG, Leith JM. Ankle fractures in diabetics: complications of surgical management. J Bone Joint Surg. 1998;80B:689-692.
27. Bibbo C, Lin SS, Beam HA, Behrens FF. Complications of ankle fractures in diabetic patients. Orthop Clin North Am. 2001;32:113-133.




