Article
Identifying Shoulder Pain in Older Patients: The History, Physical Examination, and Testing
Shoulder pain has many causes: tendinopathy, impingement, rotator cuff tear, adhesive capsulitis ("frozen shoulder"), and arthritis. This review describes tests that can help narrow the differential diagnosis.
Shoulder pain, the third most common musculoskeletal complaint in primary care physicians' offices, often occurs in older patients-it has its peak incidence in the fourth to the sixth decades of life.1 Common shoulder conditions in this age-group include rotator cuff tendinopathy, impingement, rotator cuff tear, adhesive capsulitis ("frozen shoulder"), and glenohumeral (GH) arthritis. Diagnosis can present a unique challenge because the shoulder joint is complex and shoulder pain has a broad differential.2 In addition, older patients who present with shoulder pain have issues and concerns different from those of younger patients.
For example, the differential diagnosis for shoulder pain in a younger patient is more likely to include shoulder instability, traumatic and atraumatic shoulder dislocation/subluxation, and symptomatic labral pathology. Those in the older population are more likely to have an acute rotator cuff tear, particularly after a fall onto the shoulder; a chronic, degenerative rotator cuff tear; or shoulder arthritis.
Management of shoulder pain in older patients also involves different considerations. Treatment often is based on the patient's age, activity level, level of function, and overall health status. A very active older adult may have a greater need for surgery for a rotator cuff tear, because of pain and functional limitation, than someone of the same age who is not so active or in poor health, where a longer trial of therapy may be warranted.
In this 2-part article, we describe our approach to identifying shoulder pain in older patients. This first part focuses on the use of historical clues, a thorough physical examination, and testing to help narrow the differential diagnosis. In the second part, to appear in an upcoming issue of this journal, we will discuss interpretation of clinical findings and treatment
options.
THE HISTORY
In older patients who present with shoulder pain, the history is a crucial element in creating a differential diagnosis. Start with open-ended questions, and avoid questions that may be leading. Recognizing the patient's age is important because doing so often influences the nature of the questions and helps determine your overall impression and approach to management. Ask as many questions as needed to gain a full understanding of the patient's hobbies, sports or other activities and level of participation, goals and expectations, and hand dominance.
Understanding hand dominance helps in the evaluation of strength because there may be subtle side-to-side weakness on the nondominant side. That side also may have less muscular hypertrophy, rather than asymmetry. There also may be a different arc of motion with increased external rotation on the dominant side and increased internal rotation on the nondominant side.
Asking about pain
In exploring the patient's history, ask about the location, quality, and duration of pain, as well as associated signs and symptoms. If there was an inciting event, ask for as much detail as possible about it. Determine whether there are any mechanical symptoms (eg, locking, catching, and instability).
Night pain is another symptom worth noting, and learning details about it may be helpful. Resolution of the pain experienced at night can be a useful indicator of a patient's response to treatment.
A patient having difficulty with simply lying down may suggest impingement, because the loss of gravity and the weight of the patient's arm may reproduce symptoms. If symptoms are positional, consider acromioclavicular (AC) pathology that is aggravated by placing increased weight on that joint. Pain resulting from adhesive capsulitis also may be positional because any movement of the patient's shoulder increases pain.
In addition, investigate whether there has been any previous injury to the patient's neck or shoulder. Neck pain and pain that radiates below the elbow often are subtle signs of cervical pathology, which may be mistaken for a shoulder problem.3 If symptoms are chronic, note any changes that occurred since they first began and determine whether there has been any previous response to treatment.
Review of systems
A complete review of systems also is useful. The presence of constitutional symptoms, rash, or arthralgia would raise suspicion for a rheumatologic problem. Reports of associated chest pain; a history of high cholesterol levels, hypertension, or myocardial infarction; or a family history of coronary artery disease would create concern for a cardiac cause of the shoulder pain. The presence of nausea and intermittent abdominal pain may suggest a GI disorder, such as gallbladder disease, with pain referred to the shoulder. Thoroughness in reviewing systems and considering causes other than musculoskeletal ones helps clinicians prevent missing a diagnosis.
THE PHYSICAL EXAMINATION
Develop your own systematic approach to allow for a thorough and efficient physical examination. Before beginning, ensure that you can visualize the shoulder girdles and upper trunk adequately. Observe how the patient moves and how he or she carries the shoulders with movement. Examine the patient in several positions, including standing and sitting. Perform the inspection portion of the examination from the patient's front as well as from the back. Compare the injured side with the contralateral uninjured side throughout the examination, because motion, joint laxity, and strength often vary greatly from patient to patient.
Shoulder anatomy
Because the shoulder has a wide range of motions, it can be very unstable. However, the muscles, tendons, ligaments, and bony constraints in this region all play a role in providing stability.
Awareness of shoulder anatomy helps guide the physical examination. The shoulder is a complex of 4 articulations. The GH joint, the primary joint of the shoulder, has a ball-and-socket configuration with anatomy resembling a large golf ball on a small tee or a ball balanced on the nose of a seal.4 The other 3 articulations that make up this complex are the scapulothoracic, AC, and sternoclavicular (SC) joints. The only true articular attachment of the shoulder to the axial skeleton is the SC joint.
Inspection
On examination, look for the presence of obvious deformities of the bones or soft tissues, including muscle atrophy; scars; skin discoloration; erythema; ecchymosis; swelling; and venous abnormalities. Ask the patient to sit or stand as you observe him while he raises/forward elevates and lowers/extends his arms.
In particular, look for any side-to-side asymmetry in scapular motion posteriorly. Scapular winging, or dyskinesia, indicating dysfunction of the muscles that help stabilize the scapula, has multiple causes but could support a diagnosis of internal shoulder derangement.5
Pain in the shoulder may cause reflex inhibition of surrounding muscles as a protective mechanism. This limits contraction of the muscle, which limits motion and may result in decreasing pain; however, this also may lead to muscle imbalances and scapular dyskinesia. With scapular dyskinesia, and especially with scapular winging, one must also recognize that this could result from muscle fatigue, direct trauma, or nerve injury.
Palpation
The next step is to ask the patient to show you where he is experiencing most of the pain by pointing to the location with 1 finger. Then proceed to palpation, leaving the painful areas for last. Develop your own organized method to include common areas of pathology and generators of pain, such as the SC joints, clavicles, AC joints, coracoids, biceps tendons, GH joint lines, scapular spine, cervical and upper thoracic vertebrae, and muscles (eg, deltoids, trapezia, levator scapulae, rhomboids, and cervical paraspinals).
Evaluating range of motion
Next, evaluate the range of motion of the shoulders bilaterally and of the neck. For the neck, assess flexion, extension, rotation, and lateral flexion. For the shoulder, the most important motions to evaluate functionally are forward elevation, internal rotation, and external rotation.
As the patient raises his arms, watch for shoulder "hiking" (predominantly using the upper trapezius in a shrugging motion to help elevate the arm) as he is performing forward elevation or abduction. Hiking could be an indication of weakness or dysfunction of the rotator cuff.
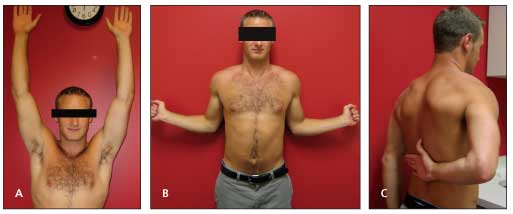
Figure 1 – Range of motion testing is shown with a demonstration of forward elevation (normal, about 170°) (A). Testing with the patient's arms at the side demonstrates the extent of external rotation (normal range, 45? to 90°) (B). This testing demonstrates internal rotation (normal in men, T9; in women, T7) (C). If the patient cannot reach the midline, document the nearest landmark, such as the sacroiliac joint or back pants pocket.
Document side-to-side differences with range of motion. Have the patient perform range of motion first actively and then passively. If there is any limitation of active range of motion, determine whether you can passively take him to within the normal range. Comparing the involved side with the contralateral uninvolved side and noting any degrees of motion that are lacking often is easier than remembering the exact degrees for normal range of motion (Figure 1).
SHOULDER-SPECIFIC TESTING
Next, continuing the examination in an organized fashion, perform shoulder-specific maneuvers. Strength testing should be done, specifically of the rotator cuff.
Manual muscle testing
Strength testing helps determine whether there is a rotator cuff tear. To evaluate the supraspinatus, conduct the supraspinatus isolation test, also known as the Jobe test. Ask the patient to forward elevate his arms to about 90° with elbows extended and then abduct his arms to about 30° anterior to the true coronal plane. Have him point his thumbs downward and resist as you apply downward pressure. Weakness noted during this test may signify true muscle dysfunction and rotator cuff pathology or muscle inhibition resulting from pain.
For the infraspinatus and teres minor muscles, test the patient's strength of external rotation. Ask him to flex his elbows to 90° and, with his elbows at his side, externally rotate as you provide resistance. Isolation of the subscapularis is difficult. Resisted internal rotation with the arm by the side and the elbow flexed to 90° is a good screening test for weakness. Further provocative testing often is needed to discern whether there is a tear of the subscapularis.
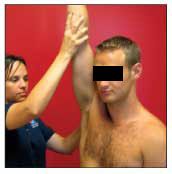
Figure 2 – The Neer sign is used to evaluate for impingement. The examiner elicits the sign by passively flexing the patient's shoulder to maximal forward elevation with 1 hand while stabilizing the patient's scapula with the other.
More provocative testingImpingement. The examiner elicits the Neer impingement sign by passively flexing the patient's shoulder to maximal forward elevation with 1 hand while stabilizing the patient's scapula with the other (Figure 2). The test result is abnormal if pain is reproduced at maximum forward flexion.
An additional evaluation, the Neer test, may be performed by first eliciting a Neer impingement sign and then injecting lidocaine into the subacromial space. After the injection, if there is temporary pain relief with the Neer impingement sign maneuver, this test result is considered to be positive (abnormal).
The Hawkins impingement reinforcement test is performed by asking the patient to forward flex his shoulder to 90° with his forearm parallel to the floor. The examiner then internally rotates the patient's shoulder while it is in this position; pain elicited with this test is considered an abnormal result (Figure 3).

Figure 3 – In the Hawkins impingement reinforcement test, the patient is asked to forward flex his shoulder to 90° with his forearm parallel to the floor. The examiner then internally rotates the shoulder. Pain elicited with this maneuver is considered an abnormal test result.
Rotator cuff injury tests. To evaluate supraspinatus muscle integrity, use the supraspinatus isolation test described above. The "empty can" version of this test (thumb in a down position) is used most often. In 1 study, however, the "full can" version (thumb in an up position) was shown to have similar accuracy in detecting a rotator cuff tear if weakness is used to define an abnormal test result.6
Isolation of the subscapularis with strength testing can be difficult. Two of the frequently used maneuvers for strength testing are the lift-off test and the belly press. The lift-off test is performed by asking the patient to reach behind his back and push his hand off his back against resistance (Figure 4). The belly press is done by having the patient flex his elbow to 90° at his side and place his hand on his abdomen; he then is instructed to press his hand down against his abdomen while the examiner attempts to lift the hand off. The belly press is particularly helpful for evaluating patients who cannot reach behind their backs because of pain and dysfunction.

Figure 4 – The lift-off test against resistance is used to evaluate subscapularis strength. Another option is to simply document the patient's ability to perform the lift-off maneuver without resistance.
Isolation of the infraspinatus and teres minor muscles is difficult because they perform similar functions. The test described in the manual muscle testing section above is a good screening tool. An additional component of strength testing is the external rotation lag sign, which involves the examiner externally rotating the patient's shoulder held at 20° of elevation in the scapular plane with the elbow in 90° of flexion. The examiner maintains support at the elbow but releases the wrist and asks the patient to maintain his arm in this fully externally rotated position. If the patient cannot do so, concern should be raised for a tear of 1 or both of these muscles.
The drop arm test is performed by asking the patient to fully abduct his arm actively or having the examiner passively abduct the arm maximally and then releasing the arm and instructing the patient to slowly lower the arm back to his side. The test result is abnormal when, during the process of lowering the arm, the patient loses control and the arm suddenly drops to his side (this often occurs at about 70° to 100° of abduction); this result usually indicates a large rotator cuff tear.
Pain in the midranges of shoulder abduction, which typically eases at the extremes of motion, is defined as a painful subacromial arc. Evaluation of a painful arc is started by asking the patient to sit or stand. The examiner then passively elevates the patient's arm to 180°. The arm then actively descends in the abduction plane. The "arc of pain" sign is present when the pain is minimal at full elevation, increases in intensity as the arm descends to 90° of abduction, and is maximal between 70° and 120° of abduction. The presence of the sign indicates the possibility of impingement or a rotator cuff tear.
Acromioclavicular joint pathology. The cross-chest adduction test, used to evaluate pathology of the AC joint, is performed by passively bringing the patient's arm into maximal adduction across his chest. When performing this test, keep 1 hand on the patient's AC joint; if pain is reproduced, ask the patient whether he is experiencing pain at the AC joint where your fingers are or in a different location. This test may elicit pain that has other causes, but a test result that suggests AC joint pathology indicates pain at the AC joint.
The O'Brien, or active compression, test may indicate an injury to the glenoid labrum if pain deep in the shoulder is reproduced; it could indicate AC joint pathology if pain is sensed over the AC joint during the test. This maneuver is performed by asking the patient to forward flex his shoulder to 90° with the elbow extended. The arm is then brought about 15° toward the midline, and the patient points his thumb downward. The patient is then asked to resist a downward force applied by the examiner.
If pain is noted, ask the patient to indicate where he is feeling the pain. Pain over the AC joint should raise suspicion for AC joint pathology. Pain deeper in the shoulder increases the possibility of labral pathology. If this is the case, continue with the second portion of this test, which is to have the patient then point his thumb upward, repeating the above maneuver. Improvement of the deep shoulder pain in this thumb-upward position is considered a positive test result for labral pathology.
The O'Brien and other tests at the shoulder may load the AC joint and recreate pain. Therefore, it is always important to ask the patient where all of the tests produce pain.
Biceps tendinopathy. The Speed test is performed by asking the patient to forward elevate his arm to 90° with his elbow fully extended. The examiner then places his hand on the patient's forearm. The patient is asked to forward elevate his arm while the examiner applies resistance.
If pain is reproduced over the long head of the biceps tendon, the result is considered abnormal and suggests pathology associated with the biceps tendon. A patient complaint of pain with this test that is deeper in the shoulder raises concern for possible labral pathology.
Neurovascular examination
Cervical pathology, including nerve impingement resulting from a herniated disk or osteophytes resulting from arthritis, cervical syrinx, or stenosis could cause radicular, or referred, pain to the shoulder. Brachial plexus injury or a labral cyst could cause nerve impingement, particularly at the spinoglenoid notch, which also could cause shoulder pain and abnormalities on examination. Therefore, performing a neurovascular examination is an important part of the physical examination for all patients with shoulder pain.
The vascular examination consists of palpating peripheral pulses bilaterally and evaluating capillary refill. If thoracic outlet syndrome is suggested by any symptoms, such as swelling in the arm, cyanosis, paresthesia, and temperature changes, also consider performing the Adson, the Modified Roos, or other maneuvers.
Document sensation, which can be done with light touch or pinprick. If there are abnormalities, a more detailed sensory examination will be needed. Test biceps, triceps, and brachioradialis reflexes (Table). Perform a Spurling maneuver (extension, rotation, and lateral bending of the neck to the involved side with an axial load applied). The Spurling maneuver evaluates for a cervical nerve root disorder. The test result is considered positive if radicular symptoms, such as shoulder or arm pain or numbness, are reproduced.
Strength testing is another important component of this portion of the examination. Test the strength of the patient's biceps and triceps, wrist flexors and extensors, and grip. Depending on which symptoms are present, consider performing the Phalen or Tinel test at the wrist for carpal tunnel syndrome or at the elbow for cubital tunnel syndrome, respectively, particularly if there is a component of numbness or tingling in the hands.
CONCLUSION
A thorough history and physical examination are helpful, but no one test is sensitive or specific enough to make a conclusive diagnosis. Part 2 of this article will address interpretation of clinical findings.
References:
References1. van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis. 1995;54:959-964.
2. Stevenson JH, Trojian T. Evaluation of shoulder pain. J Fam Pract. 2002;51:605-611.
3. Woodward TW, Best TM. The painful shoulder, part I: clinical evaluation. Am Fam Physician. 2000;61:3079-3088.
4. Kibler WB, Murrell GA. Shoulder pain. In: Brukner P, Khan K, eds. Clinical Sports Medicine. 3rd ed. Sydney, Australia: McGraw-Hill; 2007:243-288.
5. Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26:325-337.
6. Itoi E, Kido T, Sano A, et al. Which is more useful, the "full can test" or the "empty can test," in detecting the torn supraspinatus tendon? Am J Sports Med. 1999;27:65-68.




