Article
Imaging Technique May Lead to Better Diagnoses in Rheumatoid Arthritis
Author(s):
Fluorescence optical imaging, which enables visualization of inflammation in the hands in rheumatic joint diseases, correlates with ultrasound as a validated and well-established imaging technique in daily rheumatological practice, say researchers writing in Arthritis Research & Therapy this month.
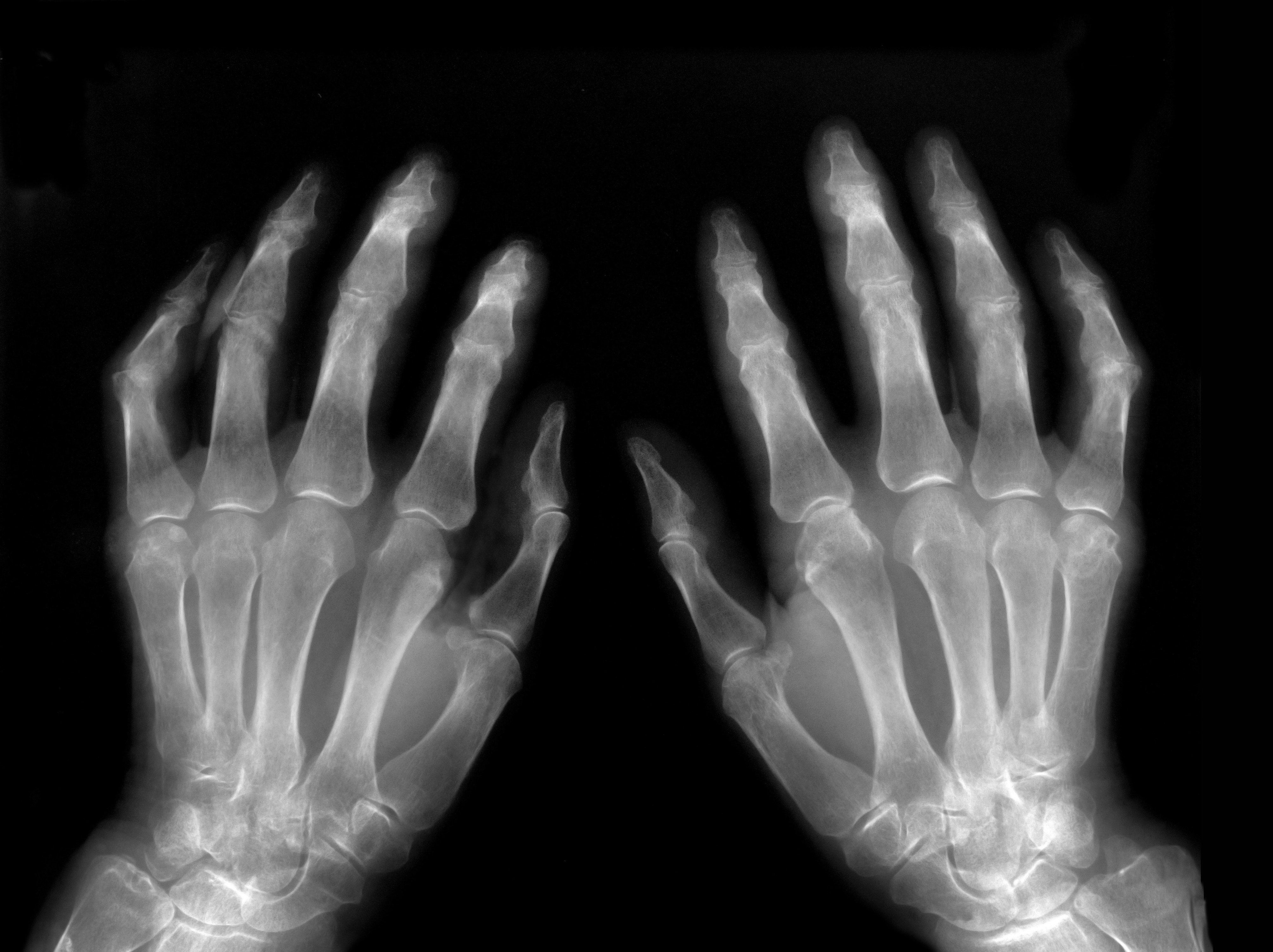
(©DarioSabljak, AdobeStock,2369226)
Fluorescence optical imaging, which enables visualization of inflammation in the hands in rheumatic joint diseases, correlates with ultrasound as a validated and well-established imaging technique in daily rheumatological practice, say researchers writing in Arthritis Research & Therapy this month.
The non-ionizing technique that examines both hands in one session of six minutes has been shown to detect inflammation in clinical studies of the joint regions of both hands, but there is a lack of long-term follow-up data.
“This present study is the first one describing the changes of fluorescence optical imaging in a homogeneous cohort of patients with early and active rheumatoid arthritis over a period of 12 months under antirheumatic therapy,” wrote the authors, led by Sarah Ohrndorf, M.D., of Charité-Universitätsmedizin Berlin in Germany.
A total of 35 patients (24 females) with a mean age 53.3 years were investigated clinically by DAS28, tender joint count and swollen joint count, and by fluorescence optical imaging in phases one through three and PrimaVistaMode before therapy change and after 12 months. The fluorescence optical imaging activity score (FOIAS) was calculated based on individual joint scores from zero to three in 30 joints per patient, adding up to a sum score (0–90).
Results showed reduction of FOIAS in phase one from baseline (median 5.0, IQR 24.96) to follow-up (median 1.0, IQR 4.0) in all patients (p = 0.0045), both in responders and non-responders according to DAS28. Statistically significant reductions over 12 months were found for median DAS28 5.61 to 3.31, tender joint count 7.0 to 1.0, and swollen joint count 5.0 to 1.0 (each less than 0.001). Meanwhile, 46 percent of the patients achieved a clinical response after one year of antirheumatic therapy, and 31.4 percent of patients achieved remission of DAS28 less than 2.6.
“A significant change of fluorescence optical imaging phase one was also observed in non-responders, so we cannot objectively deduce a therapy response of phase one.
“The significant reductions in phase one also in non-responders probably show a more objective reduction of inflammation by fluorescence optical imaging, while the clinical non-response can also depend on individual person-related (i.e., psychological) factors which may lead to elevated global disease activity on VAS,” the authors wrote.
No significant correlations were found between the FOIAS change in phase one and DAS28, tender joint count, or swollen joint count, and were weak to moderate correlations were found between the other phases and clinical outcomes.
At baseline examination, strong correlations were found between all fluorescence optical imaging phases and the ultrasound parameters, especially tenosynovitis in power Doppler ultrasound. The strongest correlations were found for fluorescence optical imaging phase two at both baseline and after 12 months of therapy, but phase one only showed a positive correlation with synovitis in greyscale ultrasound after 12 months follow-up.
“The low correlations of phase one with ultrasound at month 12 may indicate that there was no or only a small amount of acute inflammation after one year of intensive therapy, whereas the greyscale ultrasound synovitis findings can persist. Fluorescence optical imaging phase one is probably a reflection of acute inflammation,” the authors wrote.
REFERENCE
Anne-Marie Glimm, Lisa Ines Sprenger, Ida Kristin Haugen, et al. “Fluorescence optical imaging for treatment monitoring in patients with early and active rheumatoid arthritis in a 1-year follow-up period.” Arthritis Research & Therapy. September 18, 2019. doi: 10.1186/s13075-019-1989-5.




