Article
Initiating Treatment for Hepatitis C Genotype 1 Before Progression to Cirrhosis May Reduce Liver Complications
Author(s):
Watchful waiting in patients with chronic hepatitis C (HCV) genotype 1 infection may increase the number of advanced liver disease cases, according to a poster presented at the 2013 American Association for the Study of Liver Disease (AASLD) meeting held in Washington, DC.
Watchful waiting in patients with chronic hepatitis C (HCV) genotype 1 infection may increase the number of advanced liver disease cases, according to a poster presented at the 2013 American Association for the Study of Liver Disease (AASLD) meeting held in Washington, DC.
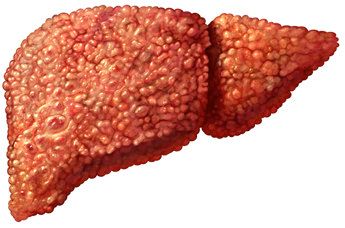
Zobair Younossi, MD, a physician at the Center for Liver Diseases at Inova Fairfax’s Department of Medicine, reported the results of a decision-analytic model for chronic HCV genotype 1 patients who are mono-infected and treatment-naïve. Using that model, Younossi and co-authors found that liver disease complications more than tripled when HCV treatment was initiated after cirrhosis was present.
In light of the growing population of HCV-infected individuals, determining the effectiveness of initiating treatment before progression to cirrhosis has important economic and quality-of-life (QOL) implications. The poster authors reported that once progression to cirrhosis has occurred, the risk of decompensation rises from just 5% in the first year to 30% after 10 years in the cirrhotic state. In addition, the risk of hepatocellular carcinoma (HCC) increases as the years of cirrhosis increase, at an annual rate of a 1% to 4% increase. Finally, response to treatment as measured by sustained virologic response (SVR) is higher among patients without cirrhosis, as compared to those who are transitioning to the final phase of chronic liver disease.
Using a state-transition model, the poster authors compared two treatment strategies: Beginning antiviral treatment in patients with no cirrhosis (determined by METAVIR fibrosis scores of F0-F3), and initiating antiviral treatment in individuals with progression to cirrhosis (METAVIR fibrosis score of F4). The state-transition model was structured to include 6 health states with annual transition points. Those health states consisted of no cirrhosis, compensated cirrhosis, decompensated cirrhoses, HCC, liver transplant, and death. For the purposes of their model, the researchers assumed that patients achieving SVR were cured and post-transplant patients retained that health status throughout their lifetimes. Transition to death could occur from any health state, and each health state had associated health risks for mortality.
The cirrhotic and non-cirrhotic cohorts were modeled by using data from clinical trials. Included in the initial decision tree were 4 treatment regimens: Sofosbuvir (SOF) in combination with pegylated interferon alfa and ribavirin (PR) for 12 weeks; telaprevir (TVR) plus PR for 24 to 48 weeks; boceprevir (BOC) plus PR for 28 to 48 weeks; or PR for 48 weeks. The probabilities for health-state transitions were derived from available medical literature, while the rates for adverse events, discontinuation, and SVR were obtained from the clinical trials used for analysis in this study. Treatment efficacy and cases of complications from liver disease were also calculated.
According to the poster authors, SVR rates were improved across all treatment regimens after initiation in patients without cirrhosis. Strikingly, cases of complications increased more than 3-fold in the cohort of patients who had compensated cirrhosis when treatment was initiated, as compared to patients without cirrhosis.
Overall, the SOF+PR regime showed the most favorable health outcomes, as that group had the highest overall SVR rates and the lowest overall number of cases of complications of liver disease, both in individuals with and without cirrhosis at initiation of treatment.
The authors acknowledged the study’s limitations, which included those typically associated with pharmacoeconomic models that use the best available data to project lifetime or long-term impact of a branching decision tree on individuals in various disease states. Additionally, the clinical trial data used for this decision-analytic model were obtained in a controlled state, rather than a real-world environment, and meta-analyses of SOF plus PR directly compared to the other treatment regimens are not currently available.
The authors disclosed that their study was funded by Gilead.




