Article
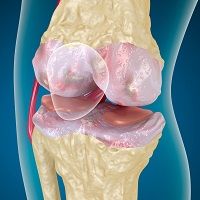
Injectable Bioactive Gel Heals Cartilage and Stops Osteoarthritis
Author(s):
With the potential for knee injuries and surgeries to results in arthritis, researchers are in the midst of developing a way to manipulate the body's cartilage to regenerate itself.
With the potential for knee injuries and surgeries to results in arthritis, researchers are in the midst of developing a way to manipulate the body’s cartilage to regenerate itself.
An orthopedic research team from the University of Iowa (UI) created a bioactive hydrogel that proved to generate new cartilage in damaged areas. Not only do their findings help patients after injury, but the gel seems to slow or prevent the development of osteoarthritis and the need for a knee replacement.
“There's really no cure for osteoarthritis except for total joint replacement, which is not particularly suitable for younger patients because the artificial joints wear out and need to be replaced multiple times," James Martin, PhD, assistant professor of orthopedics and rehabilitation at UI, said in a news release.
For quite some time it was assumed that cartilage could not repair itself, however, the team’s previous research revealed that precursor cells in normal cartilage could mature into new tissue. Documented in Arthritis and Rheumatology, the custom-made bioactive gel “can repair cartilage damage, regenerate stronger cartilage, and hopefully delay or eliminate the development of osteoarthritis and eliminate the need for total knee replacement.”
Building off of their own discovery the researchers’ new findings identified molecular signaling factors, called chondrogenic progenitor cells (CPC), which could attract the precursor cells to damaged areas. Stromal cell-derived factor 1 (SDF1) was one of the signals determined to draw out those precursor cells.
To put this understanding into action, the team created a model cartilage injury. When the hydrogel with SDF1 was injected into the holes found in the model, the precursor cells moved towards the injured spot. The cells matured into regular cartilage which repaired the area.
"This process gives us a great result," Yin Yu, one of the authors and graduate student in Martin’s lab, said. "The new cartilage integrates seamlessly with the undamaged tissue, it has normal concentrations of proteoglycans, good structural properties, and looks like normal cartilage."
The team is now focusing on the SDF1 release and growth factor in the gel. They plan to begin animal testing within the year and, provided positive results correspond, human results can start within the next 5. A novel alternative to invasive procedures to correct injury that could lead to osteoarthritis seem to be in the future.





