Article
Injection of the wrist and ulnar styloid
The wrist, a complex joint, often is involved in inflammatoryarthritis, such as rheumatoid arthritis or psoriatic arthritis. Wristsynovitis causes pain, swelling, and loss of extension. Extension of thesynovial lining may lead to synovitis of the ulnar styloid. During injectionof the ulnocarpal joint, the lidocaine and corticosteroid mixtureshould flow without resistance. Injecting air after corticosteroidinjection of the ulnar styloid creates a seal that prevents the corticosteroidfrom leaking up the needle tract into the dermal layer and creatingunsightly depigmentation. (J Musculoskel Med. 2008;25:188-189)
Surface anatomy
- Wrist. The radiocarpal and ulnocarpal joints are palpated with the palm in a pronated position. Follow the thumb and the index finger extensor tendons on the dorsum of the hand proximally and locate the depression between these tendons at the wrist by noting movement of the digits and by passively flexing/extending the wrist. Mark this area for injection of the radiocarpal joint.The ulnocarpal joint may be located dorsally and medially. On the dorsum of the wrist, the joint is palpated just distal to the ulnar styloid, again by passively extending and flexing the wrist while palpating. Alternatively, the ulnocarpal joint may be palpated as a depression on the medial (ulnar) edge of the wrist, just distal and dorsal to the ulnar styloid tip. This depression is bounded by the extensor carpi ulnaris on the dorsal side and the triquetrum distally. The arteries are avoided because they run more superficially to the volar aspect of the wrist.
- Ulnar styloid. The distal portion of the ulnar styloid is identified and palpated for local tenderness.The extensor tendon of the fifth digit is then palpated by moving the digit, and a point on the ulnar styloid away from the extensor tendon is marked for injection.
Patient position
For both injections, the patient lies supine or sits upright. The arm is extended and the palm is in a pronated position comfortably supported on a pillow or towel roll with the wrist in mild flexion.
Procedure
- Wrist (radiocarpal joint): After sterilization, inject the local anesthetic into the skin and the subcutaneous tissue overlying the wrist joint (Figure 1). Allow 1 to 2 minutes for the local anesthetic to work, then insert a 22- to 25-gauge needle perpendicular to the skin at a point just distal to the radius between the thumb and index finger extensor tendons. If bone is hit, the needle should be pulled back and slightly redirected toward the thumb. Once the needle falls into the radiocarpal space, the joint is infiltrated with corticosteroid and anesthetic agent as described above.
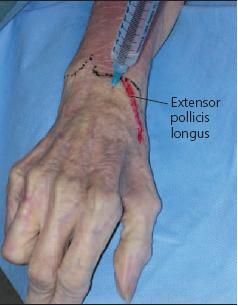
- Wrist (ulnocarpal joint): For the dorsal approach, after sterilization and injection of local anesthetic, a 22- to 25-gauge needle is inserted into a point just distal to the ulnar styloid and between the fourth and fifth extensor tendons (Figure 2). For the medial approach, a 25- gauge needle is inserted perpendicular to the skin into the depression distal and slightly palmar to the ulnar styloid, angling 10° to 15° in a cephalad direction. Once the needle falls into the space with either approach, the ulnocarpal joint is then infiltrated with the corticosteroid and local anesthetic agent.
- Ulnar styloid: After sterilization and application of local anesthetic, a 25-gauge needle is advanced toward the ulnar styloid at a 45° angle to the skin cranially. Before injection of the anesthetic and corticosteroid, the fifth digit should be flexed and extended to ensure that the tendon sheath is not being injected.
Pearls
- During injection of the ulnocarpal joint by either approach, the lidocaine and corticosteroid mixture should flow without resistance, although some pressure is required to inject through a small 25-gauge needle. Inability to depress the syringe plunger requires repositioning of the needle by a few millimeters to avoid injection into the triangular fibrocartilage complex.
- After corticosteroid injection of the ulnar styloid, you may unscrew the syringe and replace it with a syringe that contains 0.3 mL of air. Injecting air creates a seal that prevents the corticosteroid from leaking up the needle tract into the dermal layer and creating unsightly depigmentation.
Radiocarpal joint injection in a patient's right wrist is shown in this photograph.

A lateral approach to left ulnar styloid (ulnocarpal joint) injection is shown here.




