Article
The Inverted T Wave Differential Diagnosis in the Adult Patient
The natural history of the inverted T wave is variable, ranging from a normal life without pathologic issues to sudden death related to cardiac or respiratory syndromes.
The natural history of the inverted T wave is variable, ranging from a normal life without pathologic issues to sudden death related to
Figure 1A. Acute coronary syndromecardiac or respiratory syndromes. A variety of clinical syndromes can cause T-wave inversions, ranging from life-threatening events, such as acute coronary ischemia, pulmonary embolism, and CNS injury, to entirely benign conditions, such as normal variant T- wave inversions and the persistent juvenile T-wave inversion.
The normal T wave has been described to have a gradual upstroke with a more rapid downstroke in the terminal portion. This relative asymmetry may vary because many females and elderly individuals, without identifiable cardiac disease, may have symmetric T waves. The T wave is normally upright in leads I, II, and V2 to V6; inverted in lead aVR; and variable in leads III, aVL, aVF, and V1. In general, an inverted T wave in a single lead in one anatomic segment (ie, inferior, lateral, or anterior) is unlikely to represent acute pathology; for instance, a single inverted T
Figure 1B. Acute coronary syndromewave in either lead III or aVF can be a normal variant.
The interpretation of the ECG in the context of the individual patient presentation is mandatory. This interpretation strategy allows the clinician to discern among normal, potentially abnormal, and abnormal. For example, the patient with an isolated T-wave inversion in lead III in the setting of a musculoskeletal chest pain syndrome would be considered a normal variant ECG finding.
Electrophysiologic considerations: primary and secondary T-wave inversion
Figure 1C. Wellens syndrome (deeply inverted T wave)
The causes of T-wave inversions have commonly been grouped into 2 categories: primary T-wave changes and secondary T-wave changes. Alterations in the duration or morphology of the action potential, without concurrent changes in the orderly sequence of activation, are termed “primary changes.” Primary T-wave inversions are associated with benign syndromes, such as the persistent juvenile T-wave pattern and the digitalis effect, as well as morbid conditions, including acute coronary ischemic events and CNS catastrophe. Secondary T-wave changes result from aberrant ventricular activation in the context of normal action potential characteristics; examples include bundle-branch blocks, ventricular pre-excitation states (eg, Wolff-Parkinson-White syndrome), ventricular paced rhythms, and ventricular ectopic beats.
Figure 1D. Wellens syndrome (biphasic T wave)
Coronary artery disease (acute coronary syndrome, chronic ischemic syndromes)
T-wave inversions associated with coronary artery disease may result from myocardial ischemia (ie, unstable angina), non–ST-segment elevation acute myocardial infarction (NSTEMI-MI), or previous MI (Figure 1A-D). In general, inverted T waves related to acute coronary syndrome are symmetric in shape; this symmetry means that the downsloping limb is a mirror image of the upsloping limb. An important subgroup of patients with pre-infarction
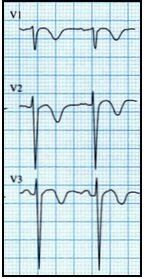
Figure 2A. Pulmonary embolism angina (ie, unstable angina) can present with significantly abnormal T-wave inversions-either symmetric, deeply inverted T waves or biphasic T waves in the precordial leads (V1, V2, and V3 in particular). In patients with this history and these ECG findings, Wellen syndrome is diagnosed, which is frequently associated with proximal left anterior descending coronary artery critical stenosis; the natural history of Wellen syndrome is anterior wall ST-segment elevation myocardial infarction. Lastly, patients with past MI can demonstrate persistent T-wave inversions as a manifestation of the MI.
Pulmonary causes
Patients with pulmonary embolism (PE) may also display T-wave abnormalities, including T-wave inversions (Figure 2A). The T-wave findings in these patients are typically shallow inversions in the inferior leads. Deeper T-wave inversions-attributed to acute right ventricular strain and occasionally seen in patients with massive PE-are generally
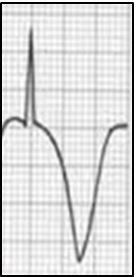
Figure 2B. CNS vascular event (subarachnoid hemorrhage)observed in the right to mid-precordial leads V1 to V4; this finding is the most specific ECG finding seen in the PE patient.
Inflammatory causes
Acute myocarditis and acute myopericarditis can present with a range of ECG abnormalities, including ST-segment elevation and T-wave inversion. T-wave inversion is not seen in all such cases of myocardial inflammatory disorders. When it is seen in these patients, T-wave inversion usually indicates a resolving process.
Neurogenic causes
There are a number of neurogenic causes of primary T-wave inversions. For example, the T waves in patients who have sustained a CNS
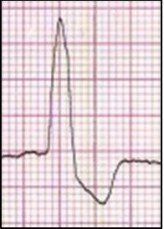
Figure 2C. Bundle-branch block (left bundle-branch block) hemorrhage or ischemic infarction are inverted with a distinctly deep, widely splayed appearance with an outward bulge of the descending limb that results in a striking asymmetry (Figure 2B). Prolonged status epilepticus is also associated with T-wave abnormalities.
Bundle-branch block and ventricular paced (implanted pacemaker) patterns
Bundle-branch block (Figure 2C) and ventricular paced (Figure 2D; implanted pacemaker) patterns produce a number of abnormalities of the ST segment and T wave. In general, leads with large positive QRS complexes will demonstrate T-wave inversions. In left bundle-branch block pattern, inverted T waves are seen in leads I, aVL, V5, and V6. In right bundle-branch block pattern,
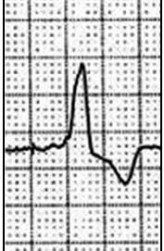
Figure 2D. Right ventricular paced rhythm from implanted pacemakerT waves are inverted in leads V1 and V2. In patients with implanted right ventricular pacemakers, inverted T waves are most often seen in leads I and aVL. The T waves are inverted in an asymmetric fashion with a gradual initial downslope and an abrupt return to the baseline.
Left ventricular hypertrophy by voltage
Left ventricular hypertrophy (LVH) by voltage pattern can be described via numerous ECG scoring systems. Perhaps the most sensitive system uses the summation of the negative component of the QRS complex in lead V1 and the positive component of the QRS complex in lead V6. If the sum is greater than 35 mm in a patient older than 35 years, then the LVH by voltage pattern is diagnosed. In patients with LVH, ST-segment/T-wave changes are encountered in approximately 70% of cases, including ST-segment

Figure 2E. Left ventricular hypertrophy by voltage deviations and abnormal T waves. Of these findings, the T wave can be inverted and is most often seen in leads with large positive QRS complexes, such as leads I, aVL, V5, and V6(Figure 2E). These inverted T waves have a gradual downsloping limb with a rapid return to the baseline. These abnormalities are related to the LVH pattern and are not suggestive of ACS.
Ventricular pre-excitation syndrome
Patients with Wolff-Parkinson-White syndrome can present with ST-segment and T-wave abnormalities as well as abnormalities of the QRS complex; these findings are termed the “pseudo-infarction findings.” For example, Q waves may be seen in leads II, III, and aVF that mimic past inferior MI. There may also be tall R waves in the right precordial leads, suggestive of a posterior wall acute MI; T-wave inversions are sometimes seen in these leads with prominent R waves (Figure 2F).
Normal variant (or benign) causes
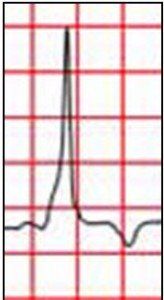
Figure 2F. Wolff-Parkinson-White syndrome
Several different clinical entities present with inverted T waves. Since T-wave abnormalities in isolation have not been studied to any extent, little epidemiologic data exist that describe their prevalence in the ECGs of both normal populations and those at risk for cardiac events. Nonetheless, an isolated T-wave inversion in a single lead is not abnormal and, in fact, is considered a normal variant finding. Other benign causes of T-wave inversion include the digitalis effect (Figure 2G) and the persistent juvenile T-wave pattern (Figure 2H). Digitalis compounds have been implicated as a cause of T-wave inversions in otherwise healthy persons. The digitalis effect refers to ECG findings that are observed with therapeutic levels of the drug-it is not a toxic manifestation. These include T-wave inversions, flattened T waves, an increased U wave, a prolonged PR interval, ST-segment depression with a distinct “scooped” appearance, and a shortened QTc interval (secondary to abbreviated ventricular action potential). Persistent juvenile T-wave inversions may appear in the precordial leads (eg, V1, V2, and V3) with an accompanying early repolarization pattern. These findings may continue into adulthood, and some patients demonstrate persistent T-wave inversions in the precordial leads.

Figure 2G. Digoxin effect
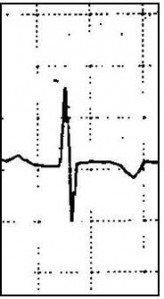
Figure 2H. Persistent juvenile T-wave pattern





