Article
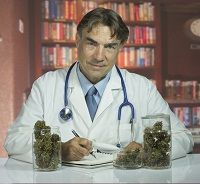
Is Medical Marijuana Safe?
Author(s):
Canadian researchers suggest that quality-controlled herbal cannabis, if used by cannabis-experienced patients as part of a monitored treatment program over one year, appears to be reasonably safe for the treatment of chronic pain.
Canadian researchers suggest that quality-controlled herbal cannabis, if used by cannabis-experienced patients as part of a monitored treatment program over one year, appears to be reasonably safe for the treatment of chronic pain.
Led by Mark Ware, BA, MBBS, MRCP(UKI), MSc, Director of Clinical Research in the Alan Edwards Pain Management Unit at McGill University Health Centre in Montreal, the study team found that patients with chronic pain who used cannabis daily for one year under close monitoring did not have an increase in serious adverse events when compared with those who did not use cannabis. The results were published online in the Journal of Pain and will serve as a benchmark study on the side effects of cannabis use in pain management.
“This is the first and largest study of the long term safety of medical cannabis use by patients suffering from chronic pain ever conducted,” said Ware, who is also an associate professor in Family Medicine and Anesthesia at McGill University. “We found that medical cannabis, when used by patients who are experienced users, and as part of a monitored treatment program for chronic pain over one year, appears to have a reasonable safety profile.”
For the prospective cohort study—named the Cannabis for the Management of Pain: Assessment of Safety Study (COMPASS)—the researchers followed 215 adults with chronic noncancer pain who were dispensed a standardized herbal cannabis product (12.5% THC) and compared them to a control group of 215 chronic pain patients who were not current cannabis users.
All participants were from one of seven clinics across Canada, located in Fredericton, Halifax, London, Montreal (two sites), Toronto, and Vancouver.
Each month for the year, cannabis was dispensed through hospital pharmacies at each site after the patients completed necessary visits and tests. Information was collected on adverse effects, lung and cognitive function, pain level, mood, and quality of life. Some also underwent complete blood panel tests of routine biochemistry, live and kidney function, and select hormone levels. The average amount of cannabis used was 2.5 grams per day, whether smoked, vaporized, or taken as edibles.
“Our data show that daily cannabis users had no greater risk than non-users (control group) to experience serious adverse events,” said Ware. “We found no evidence of harmful effects on cognitive function, or blood tests among cannabis consumers and we observed a significant improvement in their levels of pain, symptom distress, mood and quality of life compared to controls.”
It should be noted, however, that medical cannabis users did experience an increased risk of non-serious adverse events when compared with controls, including headache, nausea, dizziness, somnolence, and respiratory problems associated with smoking.
“It is important to note the limitations of the study,” added Ware. “Patients were self-selected, not randomized, and most were experienced users. So what we are seeing is that it appears to be a relatively safe drug when used by people who have already determined that it helps them. We cannot draw conclusions about safety issues of new cannabis users.”





