Article
Is Metronidazole Effective in Infants with C. difficile Infection?
Author(s):
Researchers examined the impact of metronidazole on the restoration of normal bowel habits in infants.
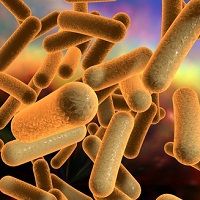
Infants can get diarrhea for a number of reasons, making reported cases of Clostridium difficile difficult to track and understand. Now, researchers believe that metronizadole is an effective treatment for the infection, according to a new report.
Researchers from the Gil Medical Center in Incheon, South Korea, observed 126 infants to determine the link between C. difficile colonization with bowel habit changes. The infants, aged between 1 and 12 months of age, had diarrhea for more than 2 weeks with conservative care. All infants were treated with conservative care at the medical center between 2006 and 2014.
While chronic diarrhea can stem from intestinal infections, intolerance to nutrients, or functional diarrhea, the researchers noted that C. difficile carrier state without apparent symptoms can be relatively common during infancy. Specifically in infants, risk factors include use of diapers, prolonged nasogastric tube insertion, and gastrostomy and jejunostomy tubes, the study authors outlined.
The infants’ mean age was about 7.5 months, and about three-quarters of them tested negative for C. difficile colonization, the researchers reported. There were no significant differences among the patients in terms of gender, age, weight at birth, gestational age, body weight, visit date, or treatment history from a primary healthcare clinic due to increased stool frequency.
The researchers determined that artificial milk formula was strongly associated with C. difficile colonization compared to infants who received breast milk. Additionally, the study authors found that infants who had received rotavirus vaccination and those with prior antibiotic use had a higher risk of colonization. The use of probiotics did not appear to have an effect on colonization, the investigators learned.
Metronidazole is used to treat C. difficile in children, partly due to its less expensive nature, the researchers added. Therefore, the researchers secondly wanted to examine the impact of metronidazole on the restoration of normal bowel habits in infants. The researchers found that metronidazole administration showed a statistically significant influence in bowel habit. However, after considering factors that influence bowel habit, such as C. difficile colonization, artificial milk formula intake, rotavirus vaccionation, use of antibiotics, and use of probiotics, the researchers found that the 2 groups (colonized and noncolonized infants) showed no significant difference.
The study authors recommend that physicians differentiate between functional diarrhea and C. difficile infection by considering the following factors: antibiotic use, exposure to enteric pathogens in daycare, growth problems, fever, rectal bleeding, and signs and symptoms of allergies. Previous studies regard infants with C. difficile as a “reservoir of C. difficile contamination,” the researchers explained, although metronidazole therapy influences bowel habit in those cases, as well.
“There was no significant association between bowel habit change and C. difficile colonization during infancy,” the study authors concluded. “On the other hand, treatment of functional gastrointestinal disorder with metronidazole during infancy was correlated with improved gastrointestinal symptoms. These findings are useful for controlling symptoms in infants with chronic diarrhea due to the possibility of controlling gut microbiota.”
The study, titled “Effect of Metronidazole in Infants with Bowel Habit Change: Irrelative to the Clostridium difficile Colonization,” was published in the journal Pediatric Gastroenterology, Hepatology & Nutrition.
RELATED COVERAGE:
Increased Incidence of C. difficile in Travelers Returning Home
Frail Patients At Risk For C. difficile Colonization
Minimizing Clostridium difficile Exposure Using Disposable Commode Pails