Article
KDIGO Updates Clinical Practice Guideline for Diabetes Management in CKD
Author(s):
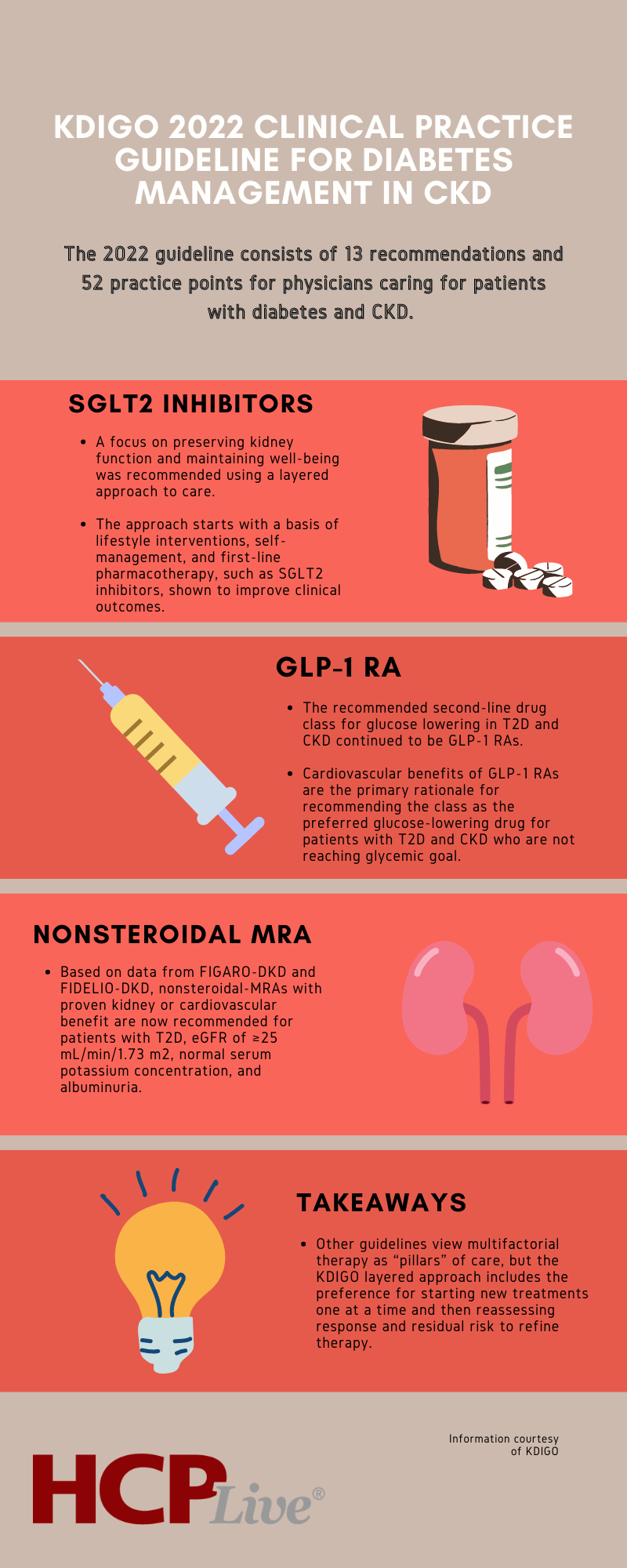
The 2022 updated guidelines includes 13 recommendations and 52 practice points for clinicians caring for patients with diabetes and chronic kidney disease.
Recently released, the Kidney Disease: Improving Global Outcomes (KDIGO) 2022 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease is an update to the 2020 guideline of the same name and advocates for a comprehensive approach to patient care.
Considering new high-quality evidence, the updates included control of multiple risk factors and a collaborative partnership among patients with chronic kidney disease (CKD) and diabetes, health care providers, and health systems to implement evidence-based recommendations that have demonstrated improved clinical outcomes.
Under a team led by Peter Rossing, Steno Diabetes Center Copenhagen and Ian H. de Boer, University of Washington, Kidney Research Institute, the overall scope, and systematic literature search for the update were unchanged from the original guideline.
A layered approach to care, lifestyle interventions were a key feature of the recommendations and new updates include therapies demonstrated to improve cardiovascular and kidney outcomes. Despite other guidelines advocating for multifactorial therapy as “pillars” of care, the KDIGO layered approach prefers starting new therapies in a singular fashion and then reassessing a patient’s response and residual risk to further refine their treatment.
The updated guideline includes 13 recommendations and 52 practice points for clinicians caring for patients with diabetes and chronic kidney disease (CKD).
“With new therapies that can reduce progression of CKD and diminish the burden of cardiovascular disease, including heart failure, health care providers should focus on preserving kidney function and maintaining well-being rather than replacing kidney function,” the study authors wrote. “The beneficial effects of SGLT2 inhibitors, nonsteroidal mineralocorticoid receptor antagonists (MRAs), and glucagon-like peptide-1 receptor agonists (GLP-1 RAs) on CKD and cardiovascular disease provide an opportunity to achieve these goals and save millions of lives, but these therapies will only benefit patients with diabetes and CKD if implemented widely.”
SGLT2 Inhibitors
The KDIGO 2020 guideline recommended SGLT2 inhibitors for people with kidney disease and an estimated glomerular filtration rate (eGFR) of at least 30 mL/min/1.73m2. The updated guideline now recommends an initiation of SGLT2 inhibitor therapy in patients with an eGFR of at least 20 mL/min/1.73 m2.
After publication of the original guidelines, 7 large trials examining the effects of SGLT2 inhibitors reported positive results and warranted the lowering of the eGFR threshold. For the guideline, the topic was moved from Chapter 4 (Glucose-Lowering Therapies in Patients with T2D and CKD) to Chapter 1 (Comprehensive Care in Patients with Diabetes and CKD).
Guidelines authors suggest the change acknowledged evidence from the seven included trials that the benefit of SGLT2 inhibitors is independent of glycemic control and the recommendation to use SGLT2 inhibitors for heart and kidney protection in patients with CKD.
A new practice point (1.3.1) suggests the recommendation for SGLT2 inhibitors is for kidney and cardiovascular protection and SGLT2 inhibitors have been shown to have safety and benefit in CKD patients, even for patients without T2D. If patients are already being treated with other glucose-lowering agents, an SGLT2i can be added to the current treatment regimen.
GLP-1 RAs
The recommended second-line drug class for glucose lowering in T2D and CKD remained GLP-1 RAs. A single new trial (AMPLITUDE-O) was added to the evidence for cardiovascular benefits of GLP-1 RAs and bolstered the hypothesis that GLP-1 RAs may also improve kidney outcomes, according to the authors.
As the cardiovascular benefits of GLP-1 RAs have been reported across strata of eGFR, the class is the preferred glucose-lowering drug for patients with T2D and CKD who are not attaining glycemic goals despite use of SGLT2 inhibitors and metformin.
A new practice point was added to suggest that GLP-1 RAs be preferentially used in patients with obesity, T2D, and CKD to promote intentional weight loss.
Nonsteroidal MRAs
A new section on the use of MRAs was included in the updated guideline. MRAs were shown to reduce residual proteinuria in individuals receiving renin-angiotensin system (RAS) inhibitors.
Smaller clinical trials reported the anti-proteinuric effects of steroidal MRAs without development of hyperkalemia, but the beneficial effects of steroidal MRAs on kidney disease progression had not been established.
Based on high-quality evidence from the FIGARO-DKD and FIDELIO-DKD trials, the use of a nonsteroidal MRA with proven kidney or cardiovascular benefit, such as finerenone, is now recommended for patients with T2D, eGFR ≥25 ml/min/1.73 m2, normal serum potassium concentration, and albuminuria despite receiving the maximum tolerated dose of an RAS inhibitor.
The recommendation is considered Grade 2A (weak or suggested) due to the availability of efficacy and safety data for only 1 drug in the class, underrepresentation of patients with moderate albuminuria, lack of data on the additive effects of SGLT2 inhibitors and MRAs, and lack of real-world data showing the safety of nonsteroidal-MRA.
Implementation
Authors noted that implementation will require community outreach efforts to make care accessible and equitable, as well as greater focus on patient preferences and priority shaping strategy.
Cost is a clear barrier to implementation. However, the team suggested that the avoidance or delay of costly kidney replacement therapy with the use of these agents may ultimately make it more cost-effective to implement new therapies, while more data is collected to support more widespread access.
“Creating a convincing case for the use of CKD therapies as part of a health system strategy for value-based care, along with lowering the cost of new therapies, is essential to translating theoretical cost-effectiveness analyses into reality,” they wrote.
“Diabetes Management in Chronic Kidney Disease: Synopsis of the KDIGO 2022 Clinical Practice Guideline Update,” was published online in the Annals of Internal Medicine.





