Article
Key Takeaways from the ADA-KDIGO Consensus Statement on CKD, with Kim Zuber, MS, PA-C, and Jane Davis, DNP
Jane Davis, DNP (Left) and Kim Zuber, MS, PA-C

Conflicting guidelines for patient care can be confusing for practitioners.
Yet, many disease states cross specialty lines and lead to multiple different answers: on age-related screening guidelines, cholesterol or lipid goals, breast cancer screening guidelines, managing heart disease risk factors and blood pressure, etc. What guidelines do we follow if the recommendations conflict? Studies have shown that practitioners are likely to follow guidelines related to experiences they have had with family, friends and/or patients.1 IE: if you have seen breast cancer in early age patients, you are more likely to recommend mammograms at an earlier age.
Diabetes is the number one cause of kidney failure and nearly 50% of all patients with diabetes will develop kidney disease.2 Even still, there are different guidelines developed by endocrine experts and those developed by kidney experts. Although they are complementary, these guidelines do not match. With this conundrum in mind, the American Diabetes Association (ADA) and the Kidney Disease Improving Global Outcomes (KDIGO) experts have come together to ‘match’ guidelines. In a recent expert consensus statement, the ADA and KDIGO combined their expertise and developed a practical, easily followed set of guidelines for patient with diabetes (Type 1 (T1DM) or Type 2 (T2DM)) and chronic kidney disease (CKD).3
Highlights of the guidelines include:
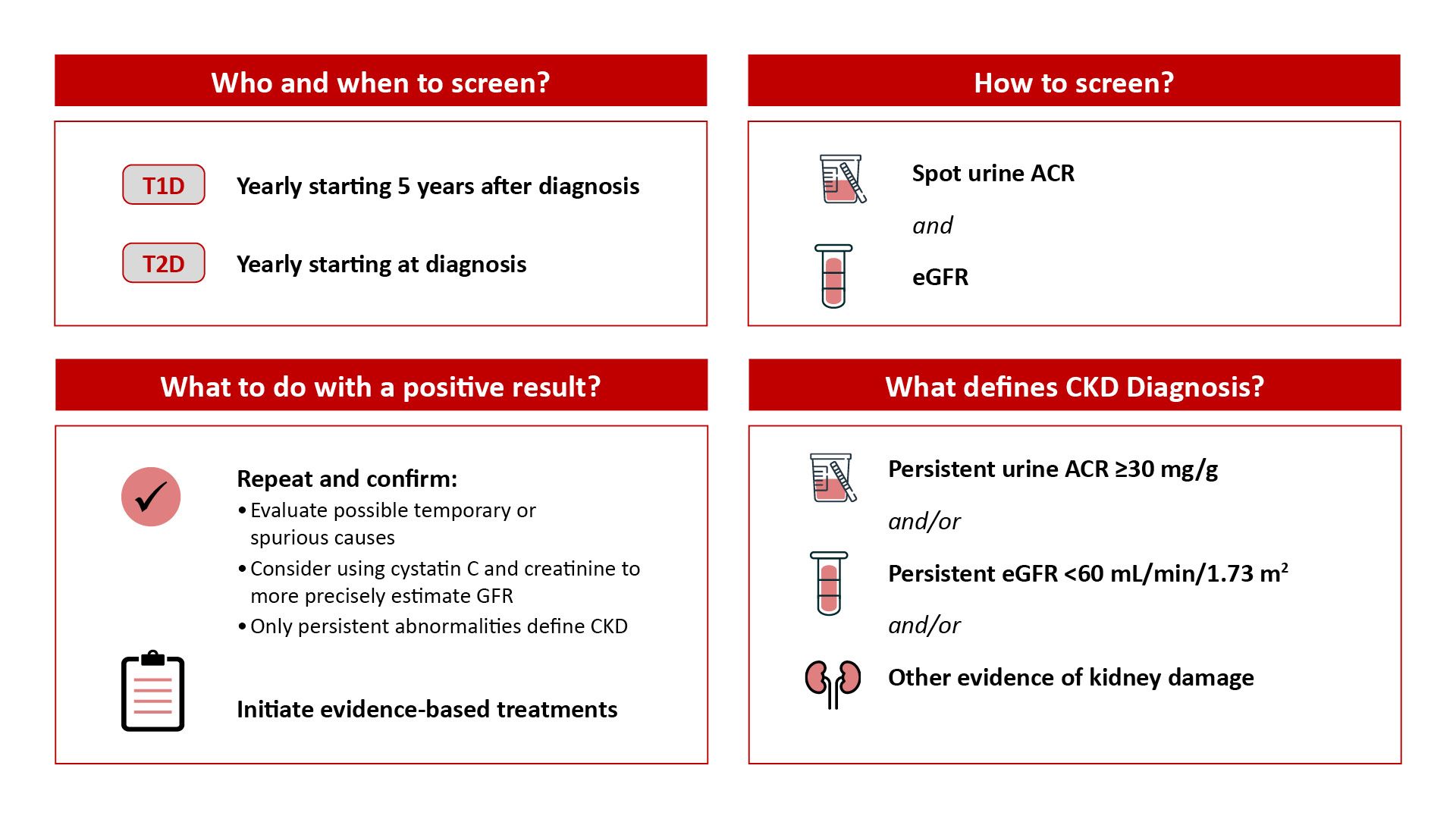
1. When and how to screen for kidney disease in a patient with diabetes3
Legend: UACR/ACR: urine albumin-to-creatinine ratio, eGFR: estimation glomerular filtration rate, T1D: type 1 diabetes, T2D: type 2 diabetes. (Source: ADA/KDIGO Guidelines)
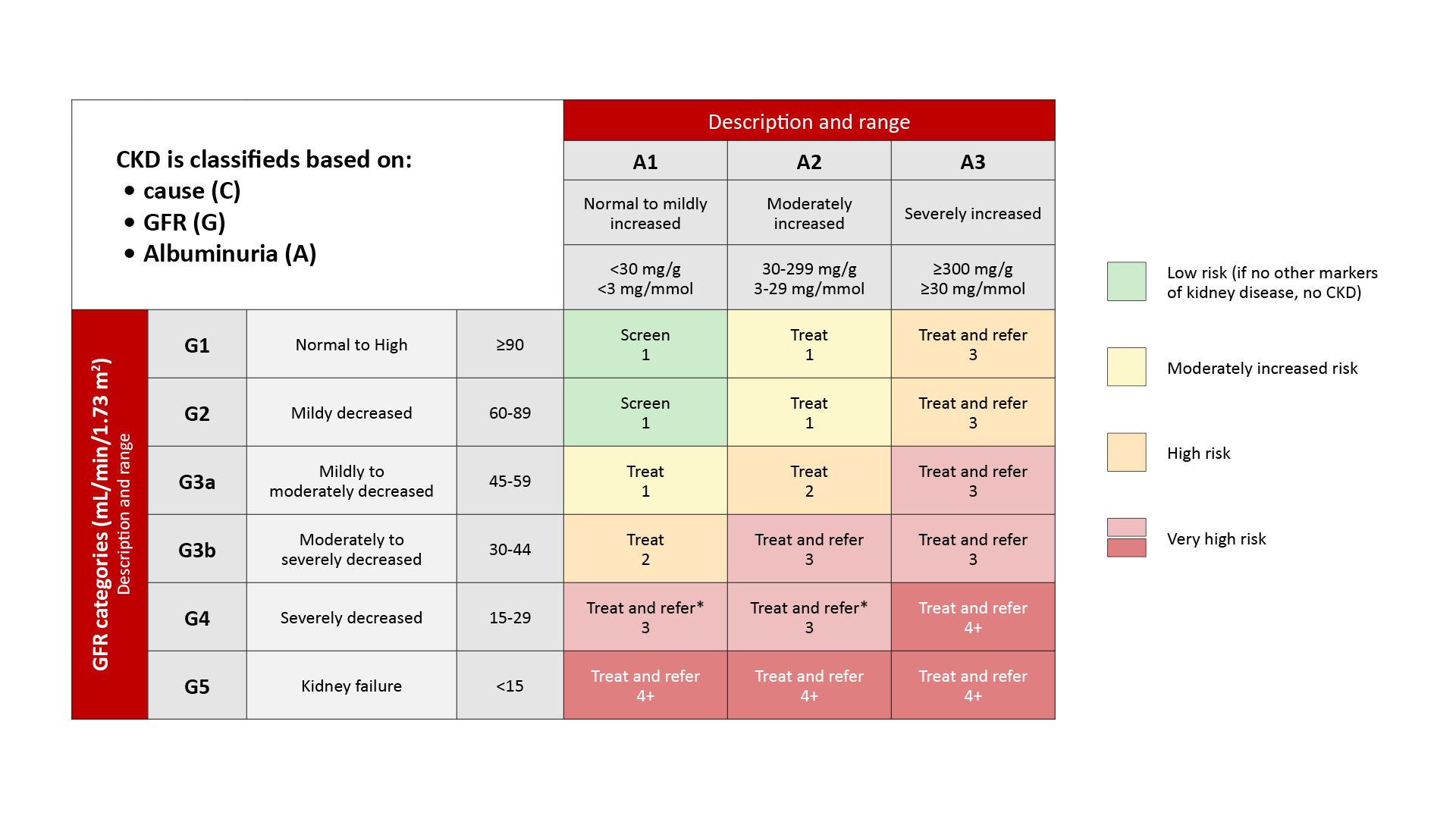
2. Agreement on the staging of kidney disease and when to refer to nephrology3
Legend: GFR: glomerular filtration rate (Source: ADA/KDIGO Consensus Statement)
3. The importance of a holistic approach for patient management
Legend: ACEi: angiotensin-converting enzyme inhibitor, ARB: angiotensin II receptor blocker, CCB: calcium channel blocker MRA: mineralocorticoid receptor antagonist, ACR: albumin-to-creatinine ratio, ASCVD: atherosclerotic cardiovascular disease, CVD: cardiovascular disease, GLP-1 RA: GLP-1 receptor agonist, PCSK9i: proprotein convertase subtilisin/kexin type 9 inhibitor, RAS: renin-angiotensin system, SGLT2i: sodium-glucose cotransporter-2 inhibitor, T1D: type 1 diabetes, T2D: type 2 diabetes (Source: ADA/KDIGO Consensus Statement)
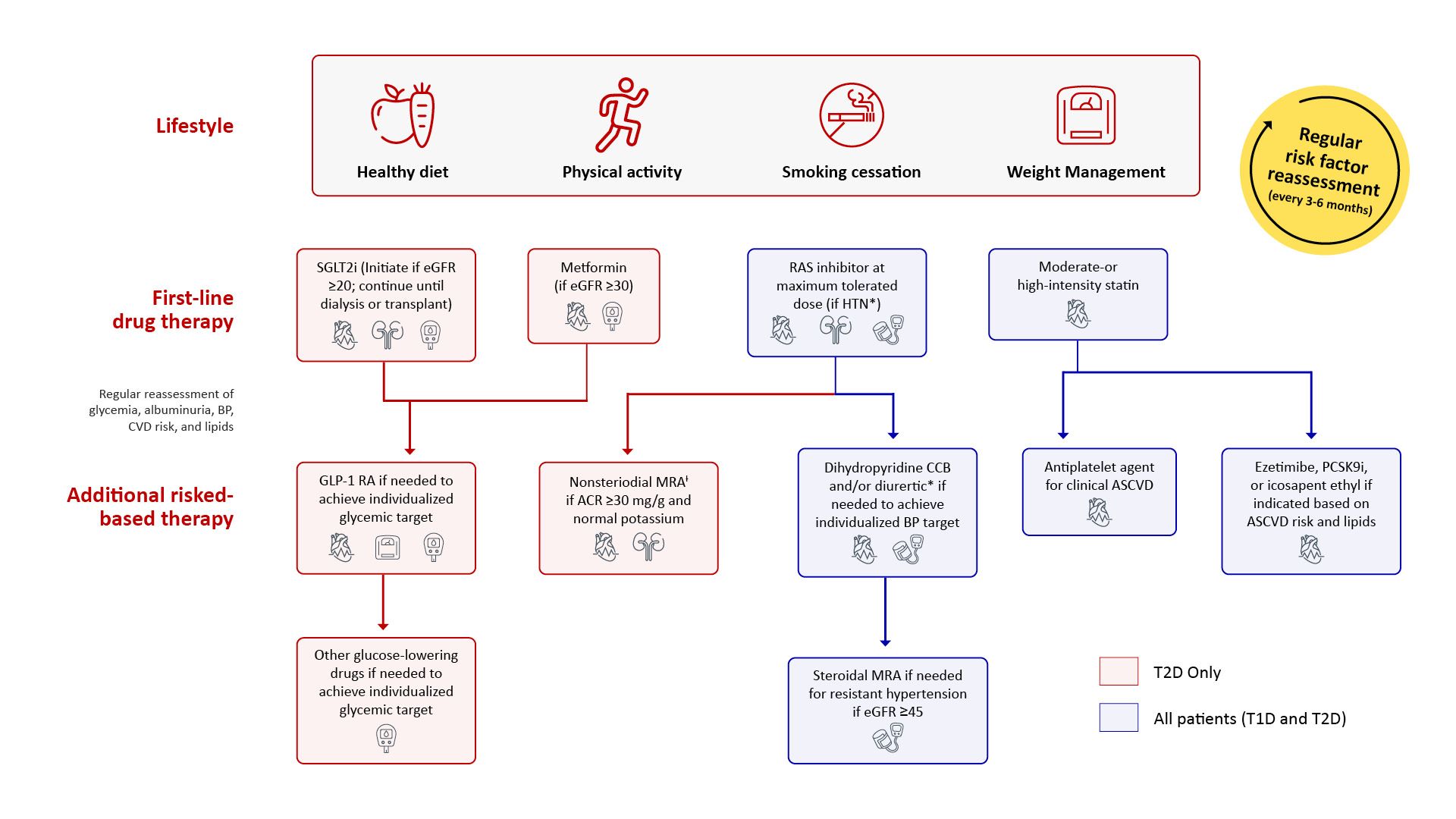
There were a couple of surprises in the updated and combined expert guidelines:
- There is still disagreement on the systolic blood pressure goal. ADA recommends a systolic goal of 130-140mmHg as an appropriate goal (depending on co-morbidities) while KDIGO recommends that 120mmHg is the appropriate goal to slow progression to kidney failure. However, both societies state the ACEi/ARBs are the initial medication of choice for hypertension management
- Both societies agree that statins are to be initiated for both patients with T1DM and T2DM
- Both societies agree that metformin is the initial medication of choice for T2DM and should be continued unless it cannot be tolerated or the patient progresses to an eGFR<30ml/min, whichever comes first
- Both societies recommend a SGLT2i for T2DM patients but in a break from the FDA package inserts, ADA and KDIGO state that the medication can be initiated at an eGFR of 20ml/min and continued when the eGFR falls below 20ml/min
- Both societies agree that the next medication of choice, for those patietns unable to take an SGLT2i, is an GLP-1 receptor agonist
- Both societies agree that for a patient with continued albuminuria and a normal potassium, a non-steroidal MRA is recommended
Managing patients with complex, multiple issues is challenging and frustrating. This is made more so when guidelines conflict.Societies coming together to combine and coordinate national guidelines is essential for quality patient care. The ADA and KDIGO have taken a major step forward in combining guidelines and hopefully this step previews future coordinated efforts between specialty organizations.
References:
- Pollack CE, Radhakrishnan A, Parker AM, et al. Association Between Physicians' Experiences With Members of Their Social Network and Efforts to Reduce Breast Cancer Screening. JAMA Intern Med. 2018 Jan 1;178(1):148-151.
- Centers for Disease Control and Prevention. Chronic Kidney Disease in the United States 2021, https://www.cdc.gov/kidneydisease/publications-resources/ckd-national-facts.html, Accessed 30Oct2022.
- de Boer IH, Khunti K, Sadusky T, et al. Diabetes Management in Chronic Kidney Disease: A Consensus Report by the American Diabetes Association (ADA) and Kidney Disease: Improving Global Outcomes (KDIGO). Diabetes Care. 2022 Oct 3:dci220027.




