Article
Low back pain management: Making the diagnosis
The main goals of low back pain management are achieving an accurate diagnosis and implementing a targeted, cost-effective treatment plan.
Low back pain (LBP) is the fifth most common reason for physician visits in the United States; about 25% of adults in the US population report LBP lasting at least 1 day in the previous 3 months.1,2 The lifetime prevalence of spinal pain has been reported as 54% to 84%.3
Although LBP is a somewhat benign condition, the cost of managing it continues to increase. Estimated total expenditures among patients reporting spine problems increased by 65% from 1997 to 2005 (adjusted for inflation)-more than overall health expenditures.4
The main goals of managing LBP are achieving an accurate diagnosis and implementing a targeted, cost-effective treatment plan aimed at pain relief and restoration of normal function. Reaching these goals requires that the clinician take a detailed history, perform an appropriate physical examination and, when they are indicated and the findings will affect the treatment plan, obtain imaging studies.
This 2-part article provides an update of approaches to LBP management. In this first part, we focus on the diagnosis. The second part, to appear in an upcoming issue of this journal, will explore the treatment options.
Assessment
A detailed evaluation of a patient with LBP is critical in establishing an appropriate diagnosis, ruling out serious medical pathology, and formulating a targeted treatment plan. The diagnosis begins with a thorough history taking and physical examination. Imaging studies and additional diagnostic tests should be performed if indicated by the history and physical examination findings, but only when they would affect the course of treatment.
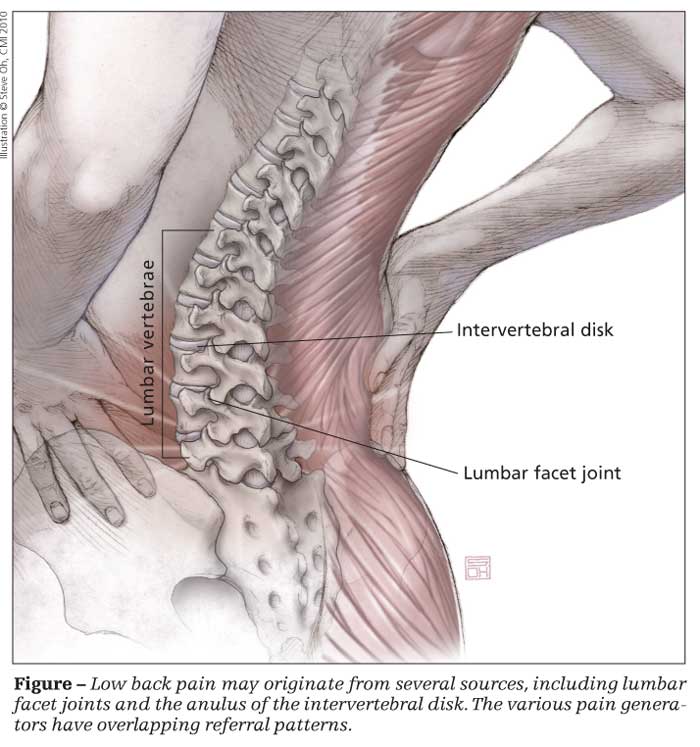
LBP may originate from several sources (Figure), including bone; joints (eg, facet joints); the anulus of the intervertebral disk; anterior longitudinal, posterior longitudinal, and interspinous ligaments; muscles; fascia; and nerve roots. These pain generators have overlapping referral patterns. The goal of the history and physical examination is to identify the probable pain generator and develop an appropriate targeted treatment plan.
History
The basic history taking for a patient complaining of LBP should include a description of the pain's location, timing, frequency, character or quality, severity, referral pattern, aggravating and alleviating factors, and associated symptoms. A pain diagram may be helpful in visually demonstrating the location and quality of the patient's complaints.5
While obtaining a history, the examiner should be aware of several “red flags” that may indicate more serious conditions that require prompt medical workup. The red flags of LBP include the following:
•Cauda equina syndrome: a change in bowel, bladd
er, or sexual function; bilateral perineal numbness or sciatica-type pain.
•Malignancy: night pain that awakens the patient from sleep, a previous history of cancer, unexplained weight loss.
•Underlying systemic disease: pain unrelieved with bed rest.
•Spinal infection: associated febrile illness.4,6
In addition, patients should be questioned about previous consultations, impressions, diagnostic testing, and treatments (including medications [tried, successful or not; adverse effects] and interventional procedures). Documenting which interventions were tried and were not successful, why they did not succeed, and which interventions did succeed is important.
Some historical information may be helpful in developing a differential diagnosis. For example, sciatica is defined as pain that originates from the lower back and radiates down below the knee. A history of true sciatica-type pain has a sensitivity of 98% and a specificity of 88% for an underlying herniated intervertebral disk.6,7
The patient should be questioned about provocative and relieving maneuvers or postures. Pain referral below the calf with sitting, forward flexion, coughing, sneezing, or bowel movements may be consistent with an underlying diskogenic cause. The history should include a detailed description of the activities that cause pain.
Psychosocial history and other factors
Pain is a subjective, individual experience. Addressing other factors that may be contributing to a patient's complaints is important. These include the patient's psychological history, work history, cigarette smoking, alcohol use, marital status, life stressors, anxiety, and expectations of treatment.
Physical examination
In combination with a detailed history, a thorough physical examination may help narrow the differential diagnosis. A comprehensive physical examination of the lumbar spine should include an in-depth evaluation of the neurological, musculoskeletal, and vascular systems. To include all key elements, the examination should be performed in sequence: inspection, palpation, range of motion, flexibility, functional and neurological assessments, and provocative maneuvers (Table).8
Diagnostic studies
Imaging studies usually should be reserved for patients who show red flags or have significant neurological findings, because it is now well known that many abnormalities may be found
on imaging studies in the asymptomatic population. In addition, there is little correlation between the findings on many imaging studies and a patient's complaint.
Plain radiographs. These are not routinely needed for most episodes of acute LBP. There is no evidence to suggest that plain radiography in patients with nonspecific LBP is associated with better patient outcomes than selective imaging.9,10 Plain radiographs may be useful for identifying underlying structural abnormalities in select patients and vertebral compression fractures in higher-risk populations.11
Bone scans. These rarely are needed in the evaluation of acute LBP. They may be useful when the history and physical examination findings suggest tumor, infection, or fracture (occult or traumatic).12,13 Bone scanning is limited by poor spatial resolution of the pertinent anatomy of the spine. Positive findings usually should be followed up by using confirmatory imaging techniques, such as MRI or CT.
MRI. This modality has demonstrated excellent sensitivity in the diagnosis of lumbar disk herniation and is considered the imaging method of choice for nerve root impingement.14 However, routine imaging with MRI or CT is not associated with better patient outcomes.10 Instead, early advanced imaging may identify radiographic abnormalities that are poorly correlated with the patient's symptoms.15
MRI should be reserved for select patients because there is a high prevalence of abnormal radiographic findings in asymptomatic persons.16 A prompt workup with advanced imaging (MRI or CT) is recommended for patients who have progressive neurological decline; a change in bowel or bladder function; or a suspected serious underlying condition, such as vertebral infection, cauda equina syndrome, or cancer with suspected spinal cord compression. MRI is preferred over CT because it does not use ionizing radiation and it provides better visualization of soft tissue, vertebral narrowing, and the spinal canal.10
MRI is not necessary for all patients who have radicular pain. It should be reserved for patients who probably will undergo invasive interventions, such as epidural injections or surgery. MRI may be helpful in determining the level of pathology in candidates for epidural injections or select nerve blocks when physical examination and electrodiagnostic examination findings are inconclusive.
CT scans. CT scanning of the lumbar spine provides superior anatomical imaging of its osseous structures and good resolution for disk herniations. When CT is used without myelography, however, the sensitivity is inferior to that of MRI. In addition, as with MRI, the frequency of positive findings in asymptomatic patients is high. CT generally is used for evaluation of bony architecture and in patients who cannot undergo MRI.14
Electrodiagnostic studies. Such studies, including nerve conduction studies, electromyography, and somatosensory evoked potentials, should be considered an extension of the history and physical examination rather than a substitute for a detailed history and thorough neurological and musculoskeletal examinations. Electrodiagnostic studies are helpful in the evaluation of patients with limb pain in whom the diagnosis remains unclear. The tests can differentiate radiculopathy from peripheral neuropathy and can help quantify the age and degree of nerve damage.5
Myelography.This involves penetration of the subarachnoid space with contrast; it usually is not indicated in acute LBP. Myelography generally is a preoperative test used with CT to provide a detailed anatomical picture of the spinal osseous elements.
Diskography. This is the radiographic examination of individual intervertebral disks after introduction of a radiopaque contrast medium into the center of the disk. It is used in the investigation of ruptured disks but rarely is necessary in the evaluation of LBP, especially within the first 3 months of treatment. Diskography generally is used to identify a symptomatic disk in patients with nonradicular LBP. To be positive, the results must include a concordant pain response.
Diskography often is used before surgical fusion is considered for unremitting back pain resulting from a symptomatic internal disk disruption. It must be used with caution because a substantial number of patients with abnormal findings improve without surgery.
In addition, in a prospective, match-cohort study, Carragee and associates17 recently concluded that modern diskography techniques result in accelerated disk degeneration, disk herniation, loss of disk height and signal, and the development of reactive endplate changes in the lumbar disk. Therefore, diskography should be reserved for select patients in a limited number of scenarios.
References:
References
1. Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain: frequency, clinical evaluation, and treatment patterns from a US national survey. Spine (Phila Pa 1976). 1995;20:11-19.
2. Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from US national surveys, 2002. Spine (Phila Pa 1976). 2006;31:2724-2727.
3. Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966-1998. J Spinal Disord. 2000;13:205-217.
4. Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems [published correction appears in JAMA. 2008;299:2630]. JAMA. 2008;299:656-664.
5. Malanga GA, Nadler SF. Nonoperative treatment of low back pain. Mayo Clin Proc. 1999;74:1135-1148.
6. Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 1992;268:760-765.
7. Barr KP, Harrast MA. Low back pain. In: Braddom RL, ed. Physical Medicine and Rehabilitation. 3rd ed. Philadelphia: Saunders Elsevier; 2007:883-927.
8. Solomon J, Nadler SF, Press J. Physical examination of the lumbar spine. In: Malanga GA, ed. Musculoskeletal Physical Examination: An Evidence-based Approach. Philadelphia: Elsevier Mosby; 2006:189-226.
9. Deyo RA, Diehl AK, Rosenthal M. Reducing roentgenogram use: can patient expectations be altered? Arch Intern Med. 1987;147:141-145.
10. Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med. 2002;137:586-597.
11. Bigos S, Bowyer O, Braen G, et al. Acute Low Back Problems in Adults. Clinical Practice Guideline No. 14. Rockville, MD: Agency for Health Care Policy and Research, US Dept of Health and Human Services; December 1994. AHCPR Publication No. 95-0642.
12. Borenstein DG, Wiesel SW, Boden SD. Radiographic evaluation. In: Borenstein DG, Wiesel SW, Boden SD, eds. Low Back Pain: Medical Diagnosis and Comprehensive Management. 2nd ed. Philadelphia: WB Saunders Co; 1995:109-135.
13. Greenspan A. Imaging techniques. In: Orthopedic Radiology: A Practical Approach. 2nd ed. New York: Gower Medical Publishers; 1992:2.1-2.11.
14. Forristall RM, Marsh HO, Pay NT. Magnetic resonance imaging and contrast CT of the lumbar spine: comparison of diagnostic methods and correlation with surgical findings. Spine (Phila Pa 1976). 1998;13:1049-1054.
15. Jarvik JG, Hollingworth W, Martin B, et al. Rapid magnetic resonance imaging vs radiographs for patients with low back pain: a randomized controlled trial. JAMA. 2003;289:2810-2818.
16. Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69-73.
17. Carragee EJ, Don AS, Hurwitz EL, et al. 2009 ISSLS Prize Winner: Does discography cause accelerated progression of degeneration changes in the lumbar disc: a ten-year matched cohort study. Spine (Phila Pa 1976). 2009;34:2338-2345.




