Article
Managing Quadriceps Strains for Early Return to Play
Quadriceps (rectus femoris) strains are common among athletes, usually after kicking or sprinting. Learn about imaging tests for diagnosis and the exercises that encourage healing and rehabilitation.
ABSTRACT: Quadriceps muscle strains occur frequently in athletes, and the rectus femoris is the most frequently injured quadriceps muscle. The mechanism of injury typically involves an eccentric contraction during kicking or sprinting. Quadriceps strains may occur at the proximal and distal musculotendinous junctions. The diagnosis is made clinically, but ultrasonography or MRI may help determine the severity of injury. Nonoperative therapy with rehabilitation exercises usually results in a return to full range of motion of the knee and hip, restoration of full strength of the quadriceps muscle, and normal function of the lower limb. In rare cases, surgical intervention may be indicated. Return-to-play decisions should be individualized for each athlete. Target goals include adequate range of motion and strength as well as tolerance of sport-specific activities. (J Musculoskel Med. 2011;28:257-262)
Quadriceps muscle strains occur frequently in athletes during sports activity.1,2 The mechanism of injury typically involves an eccentric contraction during running, jumping, or kicking in soccer, football, and other sports. The rectus femoris is the most frequently injured quadriceps muscle.
The diagnosis of quadriceps strains is made clinically, but ultrasonography (US) or MRI may help determine the severity of injury. Nonoperative therapy with rehabilitation exercises usually results in restoration of full range of motion of the knee and hip, full strength of the quadriceps muscle, and normal function of the lower limb; surgical intervention may be indicated. Return-to-play goals include adequate range of motion and strength as well as tolerance of sport-specific activities.
In this article, we discuss the anatomy involved in quadriceps strains, the clinical presentation and history, the physical examination, and the role of imaging in diagnosis. We also describe nonoperative and operative approaches to treatment, possible complications, and return-to-play decision making.
DIAGNOSIS
Although muscle strains may occur anywhere along the length of the muscle, most are seen at the musculotendinous junction in fast-twitch (type 2) fibers undergoing an eccentric contraction.3 These injuries frequently occur in the rectus femoris muscle, primarily because of its biarticular attachments.4
Fatigued muscles may be more vulnerable to strains; conditioning the muscles may be a way to prevent such injuries.5 Muscle strains have one of the highest recurrence rates of all sports injuries.6-8
Anatomy
The quadriceps muscle consists of the rectus femoris and vastus musculature (medialis, lateralis, and intermedius), all of which receive innervation from the femoral nerve. The primary function of these muscles is knee extension.9 The rectus femoris also flexes the hip because of its biarticular nature and its attachments proximal to the hip joint.
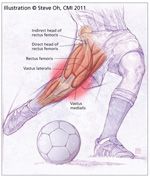
Figure 1 –
The quadriceps muscle consists of the rectus femoris and vastus musculature, which receive innervation from the femoral nerve. The direct head of the rectus femoris originates from the anterior inferior iliac spine and travels posteriorly and distally to insert by way of the common quadriceps tendon at the patella. The indirect head originates from the superior acetabular ridge and travels parallel and deep to the direct head tendon. The rectus femoris is the most frequently injured quadriceps muscle.
The direct head of the rectus femoris originates from the anterior inferior iliac spine and travels posteriorly and distally to insert by way of the common quadriceps tendon at the patella (Figure 1).10 The indirect head originates from the superior acetabular ridge and travels parallel and deep to the direct head tendon. Initially, the tendon of the indirect head lies in the medial aspect of the muscle and migrates to the middle of the muscle belly. The muscle fibers arise from the tendon and travel distally in a medial, lateral, or posterior direction to the distal tendon, which terminates in the distal third of the muscle belly.
The origin of the vastus medialis is the intertrochanteric line of the femur and the medial aspect of the linea aspera. The vastus intermedius originates at the anterolateral aspect of the femoral shaft. The vastus lateralis originates at the greater trochanter, the lateral lip of the linea aspera, and the lateral intermuscular septum. The vastus muscles coalesce with the direct head of the rectus femoris to form the common quadriceps tendon attaching to the patella.
Clinical presentation
and history
A quadriceps strain elicits an acute onset of pain in the patient’s anterior thigh during an activity that requires explosive muscle contraction; if severe, the strain results in swelling and ecchymosis. In some instances, patients describe a “pop” or tightness in the involved area. In many cases, the athlete cannot continue to compete.
Common mechanisms of injury include an eccentric contraction that occurs during various phases of kicking (back swing, ball contact, or ground contact before back swing) and deceleration before heel strike in sprinting.11 Most patients present with a loss of knee flexion or an anterior thigh mass or both.4,12-14 Distal injury to the quadriceps at the musculotendinous junction has been described frequently, usually in patients older than 40 years.15
Quadriceps strains also have been found to occur at the proximal musculotendinous junction. Hughes and associates12 recognized a pattern of rectus femoris strain injuries that consisted of an incomplete intrasubstance tear at the musculotendinous junction formed by the deep tendon of the indirect head of the muscle. MRI of the patients’ thighs revealed abnormal high signal intensity around the intramuscular tendon of the indirect head. Surgical dissection performed on 2 athletes who had chronic injury revealed gross evidence of scar tissue and fatty deposits encasing the deep, intramuscular tendon of the indirect head of the muscle.
There have been cases of proximal quadriceps avulsions in adults. A retrospective review identified 11 proximal rectus femoris avulsions in National Football League (NFL) players from 1997 to 2006.16 The injuries occurred in 2 kicking athletes and 9 nonkicking athletes. All of the athletes were treated nonoperatively; the mean time to return to play was 69.2 days.
A case report also identified proximal rectus femoris avulsions in 2 NFL kickers.17 They were confirmed with MRI, and both athletes were able to return to play with nonoperative treatment.
Why injuries occur proximally rather than distally is not known. In skeletally immature athletes, forceful flexion of the hip (eg, with sprinting or kicking) typically causes an avulsion of the anterior inferior iliac spine apophysis rather than a tear of the muscle as seen in adults.
Physical examination
On inspection, the anterior thigh usually is swollen. Pain may be elicited, or accentuated, with resisted knee extension.18
Tenderness to palpation is elicited at the proximal or distal musculotendinous junction, depending on the site of injury. There also may be tenderness in the midbelly of the muscle involved. If a palpable mass or defect is present, then a more severe injury with complete muscle rupture should be suspected. Thigh circumference should be measured to evaluate for swelling, hematoma, or defect. Acute compartment syndrome should be considered if there is tenseness of the fascial envelope surrounding the compartment and pain out of proportion to the clinical situation.19
For chronic rectus femoris strains, a palpable mass and pain with flexion may be present. However, strength and range of motion usually are the same as on the contralateral side.18
Muscle strains may be classified in 1 of 3 categories on the basis of severity: mild (grade 1), moderate (grade 2), or severe (grade 3) (Table 1).18 Differentiation between moderate and severe strains may be difficult in the first 7 to 10 days after injury, and repeated examinations may be necessary. Patients with a grade 2 or 3 strain usually cannot continue the activity they were performing. After swelling diminishes, contraction of the muscles in a grade 3 strain may reveal muscle retraction or a palpable defect.
TABLE 1
Classification of quadriceps strains
Imaging
Plain radiographs may be obtained to evaluate patients for other injuries, such as femoral fractures or avulsion injuries, particularly in the skeletally immature or adolescent population. US and MRI may be considered to assess patients for soft tissue injuries. Finlay and Friedman20 reported that US is a highly sensitive and specific method for evaluating acute quadriceps injuries. The use of dynamic US with the knee in flexion and extension helps examiners differentiate between hematoma and muscle tears. Note, however, that US images and interpretation are operator-dependent.
Many authors consider MRI to be the gold standard of imaging for muscle injuries.21-23 High signal intensity on T2-weighted images may be found at the musculotendinous junction within the quadriceps muscle.23

Figure 2 –
A sagittal MRI view shows a rectus femoris strain (arrow). In one study, injuries that involve more than 15% of the rectus femoris cross-sectional area resulted in a longer rehabilitation interval and strains longer than 13 cm also resulted in a prolonged recovery time.
Cross and associates24 reported that MRI may be used to estimate the size of a quadriceps strain and help predict the prognosis for acute quadriceps injuries. Injuries that involve more than 15% of the rectus femoris cross-sectional area resulted in a longer rehabilitation interval. Strains longer than 13 cm also resulted in a prolonged recovery time (Figure 2).
Injuries of the rectus femoris central tendon contributed to a significantly longer rehabilitation interval than injuries located in the periphery of the rectus femoris and the vastus muscles. Fluid enhancement around the central tendon, the so-called acute bull's-eye lesion (Figure 3), also revealed a significantly worse prognosis (rehabilitation interval, 26.8 days vs 9.2 days) compared with lesions found around the periphery of the rectus femoris.24
MRI also may detect rectus femoris origin injuries. In a retrospective study that evaluated MRI of these injuries, Ouellette and colleagues25 found that the majority of the injuries occur at the indirect head of the rectus femoris. They postulated that in more severe cases, there may be a progression of acute injury from the indirect head of the rectus femoris origin to the direct head.

Figure 3 –
An axial MRI view of a rectus femoris central tendon injury shows fluid enhancement around the central tendon, the acute bull’s-eye lesion (arrow). The injury has a significantly worse prognosis than lesions found around the periphery of the rectus femoris.
TREATMENT
Nonoperative
The main short-term goal of treatment is to control pain and swelling. If the patient has an antalgic gait, the use of crutches is encouraged until no limp is present. A short period of RICE (Rest, Ice, Compression, and Elevation) followed by early mobilization should be encouraged. NSAIDs also may be considered for initial treatment to decrease pain and swelling. Therapeutic US is used frequently in the management of muscle injuries; however, the data supporting this modality are inconsistent.26,27
During the initial phase of rehabilitation, eccentric contractions of the quadriceps muscle should be avoided.28 The patient is provided with a stepwise rehabilitation program (Table 2). Patients who have grade 1 strains may progress through rehabilitation more rapidly than patients who have grade 2 or 3 strains.
Isometric exercises are instituted, and patients may progress as long as they remain pain-free. When strength and range of motion improve, a patient may transition to isotonic exercises, with increasing resistance as tolerated.29
After isometric and isotonic exercises become tolerable, isokinetic exercises may be started; the focus should be on low resistance and high speeds. These exercise programs are useful because the resistance is accommodating. This allows injured athletes to work throughout a full range of motion.
A progressive running program should be initiated, starting with a slow jog and increasing to a sprint. Plyometric and jumping exercises also may be performed.
After tolerating these activities without pain and after attaining the ability to stretch the muscle as much as the healthy contralateral muscle, patients may then begin sport-specific training. Athletes involved in kicking sports may start with kicking a light ball over short distances and gradually increase to kicking a normal-weight ball over longer distances.24 Throughout the rehabilitation process, general fitness may be maintained via upper body training.
Patients may return to play after completion of a rehabilitation program. However, they should be encouraged to continue to strengthen the quadriceps.
TABLE 2
Phases of quadriceps strain rehabilitation
Operative
Indications for surgical intervention for quadriceps injuries are few. They include select cases of complete tears, persistent pain with nonoperative treatment, reattachment of displaced avulsion fractures, and large hematoma evacuation.18,28
One case report documented surgical treatment for a semiprofessional soccer player with a proximal rectus femoris rupture after 12 months of nonoperative treatment had not succeeded.11 Surgical reattachment was performed, and the patient made a full recovery and returned to sports activity at 6 months.
Irmola and coworkers30 reported on 5 cases of rectus femoris avulsions managed surgically in 4 professional soccer players and 1 hurdler. All of the athletes were operated on 18 to 102 days after the injury. Return to sports activity averaged 9 months. Two of the 5 athletes had postoperative lateral femoral cutaneous nerve palsy. In almost all cases, nonoperative treatment results in full range of motion of the knee and hip with restoration of full strength and function of the quadriceps muscle.
COMPLICATIONS
Although compartment syndrome, an acute complication, is rare, it should be recognized early to avoid irreversible damage to the lower limb. One case report described acute compartment syndrome of the anterior thigh after a quadriceps strain in a soccer player.19 The athlete’s compartment pressure measured 29 mm Hg (normal range, 0 to 8 mm Hg) in the anterior compartment, and the circumference of his thigh was 6 cm greater than that on his noninvolved side. He was able to fully return to playing soccer at 5 months after undergoing a decompressive fasciotomy.
Potential long-term complications of quadriceps strains include myositis ossificans and residual weakness. Rare after quadriceps strains, myositis ossificans results from muscular and soft tissue disruption that leads to heterotopic ossification.31 It usually is suspected with persistent soft tissue swelling and pain that does not resolve after 10 to 14 days and with healing that does not progress with adequate nonoperative treatment.29 Patients also may report increased induration and loss of motion for many weeks after the injury.32
Prevention of the formation of a hematoma initially should be attempted with RICE. If a hematoma is present, the potential for myositis ossificans should be suspected in patients with less than 120° of active knee flexion.33 In a select group of athletes with quadriceps contusions, Aronen and associates34 found that myositis ossificans occurs less frequently with immediate immobilization of the knee in 120° of flexion than with flexion as tolerated.
If myositis ossificans occurs in spite of preventive efforts, recovery of normal activity and strength still may be achieved. Patients should be treated with early motion and strength training. Surgical excision may be considered to remove the myositis ossificans if it is prominent or if it causes significant limitations in range of motion.35
We recommend immediate immobilization for patients with an acute hematoma to try to prevent myositis ossificans but we do not immobilize once myositis ossificans has developed. If the patient has myositis ossificans, we recommend gradual mobilization.
RETURN TO PLAY
The usual goal for return to play is optimal fitness with a relatively low likelihood of recurrence of injury. Recommendations for return to play typically are based only on expert opinion. There have been no randomized trials comparing rehabilitation programs.
Return to play may be advised after a patient achieves range of motion symmetrical with that on the contralateral side, isokinetic quadriceps strength within 15% of that on the contralateral side, and completion of a functional training program.18 The athlete should be observed while sprinting straight forward and while changing direction (eg, figure-of-eight) without pain or limitation. In addition, the athlete’s playing position and the time of season (ie, preseason vs play-offs) may be considered in individual return-to-play decisions.36
Orchard and Best6 suggested an approach of risk minimization rather than risk elimination. They stated that waiting for complete recovery of the muscle strain injury may be unnecessarily conservative; it decreases the rate of injury recurrence but increases overall time of missed athletic activity.
SUMMARY
Quadriceps muscle injuries may result in significant disability and loss of playing time. They are best managed nonoperatively, with a treatment program including appropriate rehabilitation exercises. The goal is to restore normal range of motion, strength, and function. Return-to-play decisions should be individualized and based on multiple factors, including the athlete's degree of injury and level of activity.
References:
References
1. Garrett WE Jr. Muscle strain injuries. Am J Sports Med. 1996;24(6 suppl):S2-S8.
2. Järvinen MJ, Lehto MU. The effects of early mobilisation and immobilisation on the healing process following muscle injuries. Sports Med. 1993;15:78-89.
3. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29:521-533.
4. Temple HT, Kuklo TR, Sweet DE, et al. Rectus femoris muscle tear appearing as a pseudotumor. Am J Sports Med. 1998;26:544-548.
5. Volpi P, Melegati G, Tornese D, Bandi M. Muscle strains in soccer: a five-year survey of an Italian major league team. Knee Surg Sports Traumatol Arthrosc. 2004;12:482-485.
6. Orchard J, Best TM. The management of muscle strain injuries: an early return versus the risk of recurrence. Clin J Sport Med. 2002;12:3-5.
7. Orchard J, Seward H. Epidemiology of injuries in the Australian Football League, seasons 1997-2000. Br J Sports Med. 2002;36:39-44.
8. Woods C, Hawkins RD, Maltby S, et al; Football Association Medical Research Programme. The Football Association Medical Research Programme: an audit of injuries in professional football-analysis of hamstring injuries. Br J Sports Med. 2004;38:36-41.
9. Armfield DR, Kim DH, Towers JD, et al. Sports-related muscle injury in the lower extremity. Clin Sports Med. 2006;25:803-842.
10. Hasselman CT, Best TM, Hughes C 4th, et al. An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Am J Sports Med. 1995;23:493-499.
11. Straw R, Colclough K, Geutjens G. Surgical repair of a chronic rupture of the rectus femoris muscle at the proximal musculotendinous junction in a soccer player. Br J Sports Med. 2003;37:182-184.
12. Hughes C 4th, Hasselman CT, Best TM, et al. Incomplete, intrasubstance strain injuries of the rectus femoris muscle. Am J Sports Med. 1995;23:500-506.
13. Raskin RJ, Rebecca GS. Posttraumatic sports-related musculoskeletal abnormalities: prevalence in a normal population. Am J Sports Med. 1983;11:336-339.
14. Garrett WE Jr. Strains and sprains in athletes. Postgrad Med. 1983;73:200-209.
15. Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg. 1981;63A:932-937.
16. Gamradt SC, Brophy RH, Barnes R, et al. Nonoperative treatment for proximal avulsion of the rectus femoris in professional American football. Am J Sports Med. 2009;37:1370-1374.
17. Hsu JC, Fischer DA, Wright RW. Proximal rectus femoris avulsions in National Football League kickers: a report of 2 cases. Am J Sports Med. 2005;33:1085-1087.
18. Waterman S. Section B: The thigh. In: DeLee JC, Drez D Jr, Miller MD, eds. DeLee and Drez’s Orthopaedic Sports Medicine. 3rd ed. Philadelphia: Saunders Elsevier; 2009:1493-1497.
19. Burns BJ, Sproule J, Smyth H. Acute compartment syndrome of the anterior thigh following quadriceps strain in a footballer. Br J Sports Med. 2004;38:218-220.
20. Finlay K, Friedman L. Ultrasonography of the lower extremity. Orthop Clin North Am. 2006;37:245-275, v.
21. De Smet AA, Best TM. MR imaging of the distribution and location of acute hamstring injuries in athletes. AJR. 2000;174:393-399.
22. Shellock FG, Fleckenstein JL. Muscle physiology and pathophysiology: magnetic resonance imaging evaluation. Semin Musculoskelet Radiol. 2000;4:459-479.
23. Speer KP, Lohnes J, Garrett WE Jr. Radiographic imaging of muscle strain injury. Am J Sports Med. 1993;21:89-95.
24. Cross TM, Gibbs N, Houang MT, Cameron M. Acute quadriceps muscle strains: magnetic resonance imaging features and prognosis. Am J Sports Med. 2004;32:710-719.
25. Ouellette H, Thomas BJ, Nelson E, Torriani M. MR imaging of rectus femoris origin injuries. Skeletal Radiol. 2006;35:665-672.
26. Rantanen J, Thorsson O, Wollmer P, et al. Effects of therapeutic ultrasound on the regeneration of skeletal muscle myofibers after experimental muscle injury. Am J Sports Med. 1999;27:54-59.
27. Wilkin LD, Merrick MA, Kirby TE, Devor ST. Influence of therapeutic ultrasound on skeletal muscle regeneration following blunt contusion. Int J Sports Med. 2004;25:73-77.
28. Best TM. Soft-tissue injuries and muscle tears. Clin Sports Med. 1997;16:419-434.
29. Järvinen TA, Järvinen TL, Kääriäinen M, et al. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33:745-764.
30. Irmola T, Heikkilä JT, Orava S, Sarimo J. Total proximal tendon avulsion of the rectus femoris muscle. Scand J Med Sci Sports. 2007;17:378-382.
31. Booth DW, Westers BM. The management of athletes with myositis ossificans traumatica. Can J Sport Sci. 1989;14:10-16.
32. Beiner JM, Jokl P. Muscle contusion injury and myositis ossificans traumatica. Clin Orthop Relat Res. 2002;403(suppl):S110-S119.
33. Ryan JB, Wheeler JH, Hopkinson WJ, et al. Quadriceps contusions: West Point update. Am J Sports Med. 1991;19:299-304.
34. Aronen JG, Garrick JG, Chronister RD, McDevitt ER. Quadriceps contusions: clinical results of immediate immobilization in 120 degrees of knee flexion. Clin J Sport Med. 2006;16:383-387.
35. Beiner JM. Muscle Contusion Injuries: Impact Biomechanics, Healing, and Treatment Aspects [medical doctorate thesis dissertation]. New Haven, CT: Yale University School of Medicine; 1997.
36. Orchard J, Best TM, Verrall GM. Return to play following muscle strains. Clin J Sport Med. 2005;15:436-441.




