Article
Meeting the challenge of chronicshoulder pain: The diagnosis
Shoulder pain is complex and difficult for even experienced clinicians to diagnose. This article reviews how to use history, simple physical tests, and imaging to distinguish rotator cuff disorders and osteoarthritis from osteonecrosis, adhesive capsulitis, labral tears, or acromioclavicular joint pathology.
Shoulder pain is a complex clinical condition, with multiple and even overlapping causes, which makes the diagnosis and treatment difficult for even the most experienced clinicians. The most common causes of chronic shoulder pain are rotator cuff disorders and osteoarthritis (OA) of the glenohumeral (GH) joint, but pain also may result from osteonecrosis; adhesive capsulitis, or frozen shoulder; labral tears; or acromioclavicular (AC) joint pathology.
In this 2-part article, we provide an update on the latest in chronic shoulder pain diagnosis and management. This first part focuses on making the diagnosis on the basis of the patient history, physical examination, and diagnostic imaging, offering primary care physicians useful information for treatment or referral to an orthopedic surgeon. In the second part, to appear in an upcoming issue of this journal, we will discuss the various nonsurgical and surgical treatment options.
Background
Chronic shoulder pain is a common complaint among patients presenting to a physician, accounting for 16% of musculoskeletal office visits.1 The annual incidence is about 15 new episodes per 1000 patients seen in the primary care setting; the peak incidence occurs in patients aged 45 to 64 years.1,2 Shoulder pain is more common in women and in patients older than 40 years than in other persons.3 The incidence of GHOA is higher in white persons than in Asian American and African American persons.
Anatomy
The shoulder is composed of 4 separate articulations: the sternoclavicular, GH, AC, and scapulothoracic joints. All may be sources of pain.
The glenoid socket is shallow, but depth and stability are enhanced by the fibrocartilaginous labrum. The labrum prevents humeral subluxation and serves as an attachment site for structures within the shoulder capsule.
The rotator cuff, largely responsible for shoulder stability, is composed of 4 muscles. The supraspinatus and infraspinatus originate on the posterior scapular fossa and insert on the greater tuberosity of the humerus. The subscapularis originates on the anterior scapular fossa and inserts on the lesser tuberosity of the humerus. The teres minor originates from the lateral scapula and also inserts on the greater tuberosity.
External rotation is accomplished through the action of the infraspinatus and teres minor; internal rotation is achieved mainly through the subscapularis. Abduction of the arm occurs through the supraspinatus and the overlying deltoid muscle. The supraspinatus tendon is most frequently injured in persons who present with shoulder pain resulting from rotator cuff disease.
History
Taking a thorough history is necessary to arrive at an accurate diagnosis. Important assessments include the patient's level of pain and functional limitations pertaining to the shoulder, as well as systemic and other joint involvement, response to medical treatment, and the presence of night or rest pain. Pain often develops gradually without the occurrence of a specific traumatic event. The patient's age and work, sports, and recreational histories also are important in the evaluation of shoulder pain because this information may help narrow the possible causes and guide further treatment.
A history of chemotherapy or corticosteroid treatment may indicate a diagnosis of osteonecrosis. The patient's response to previous treatments, including physical therapy, NSAIDs, and cortisone injections, also may influence management decisions.
Patients who present with symptoms resulting from GHOA, osteonecrosis, or adhesive capsulitis often complain of pain and decreased mobility. With rotator cuff pathology, pain tends to be the most common complaint and motion typically is preserved. The pain is aggravated by overhead motion and may be present at night or at rest. The patient also may complain of weakness and an inability to raise the arm above his or her head.
Physical examination
Physical examination of the shoulder begins with inspection and palpation. Comparing the shoulders is important, along with assessing muscle tone, symmetry, and deformity. Palpation often reveals areas of tenderness or swelling. Evaluation of active and passive range of motion of both shoulders, along with specific provocative tests of the injured shoulder, further help the diagnosis.
Localizing pain associated with OA often is difficult. Pain typically is felt deep in the GH joint; patients may have tenderness along the anterior or posterior GH joint line.
The compression rotation test may be useful in localizing pain to the GH joint. During this test, the examiner compresses the GH joint while the patient lies in the lateral decubitus position with the affected shoulder up; rotating the arm may further accentuate pain originating in the GH joint.4
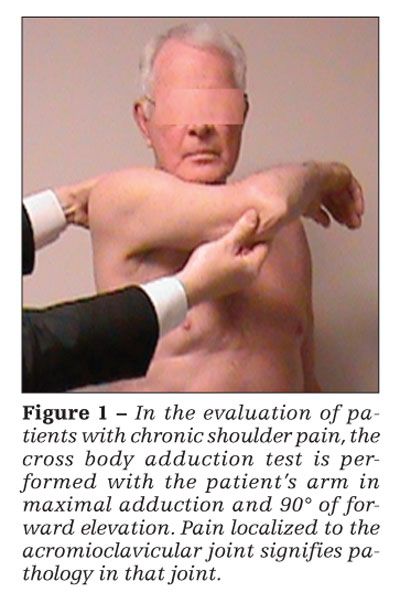
In ACOA or osteolysis of the distal clavicle, pain is localized directly over the AC joint. Increasing pain at the AC joint with passive adduction of the arm across the body is indicative of AC joint pathology (Figure 1). A diagnostic injection of lidocaine often is useful for distinguishing AC joint pain from rotator cuff pathology.5
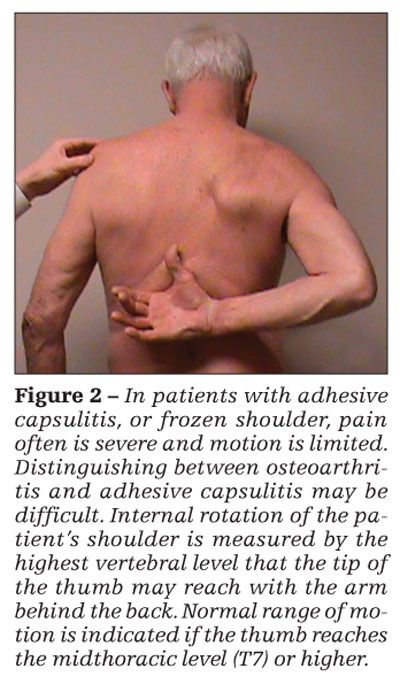
With adhesive capsulitis, pain often is severe and motion is restricted (Figure 2). Patients also experience pain along the GH joint line, particularly anterior pain. Distinguishing between OA and adhesive capsulitis may be difficult, although pain associated with the latter often is more severe and of shorter duration. Radiographic studies are important for distinguishing these diagnoses. Even with a thorough physical examination, adhesive capsulitis can be a difficult diagnosis to make and may be difficult to distinguish from shoulder pain of other causes.
In assessment of rotator cuff disease, the shoulder is inspected for signs of muscle wasting in the deltoid as well as in the supraspinatus and infraspinatus fossa. Palpation should be performed to localize the pain. Patients with rotator cuff disease most frequently present with tenderness over the greater tuberosity. Active range of motion often is diminished, with the patient unable to forward flex the arm beyond 90°; passive range of motion is preserved. Weakness may be present in the affected shoulder and may be assessed with active resistance. Difficulty with internal rotation of the shoulder indicates subscapularis tendon injury.
Provocative tests
Many provocative tests may be used to determine rotator cuff pathology. The following are the most common tests:
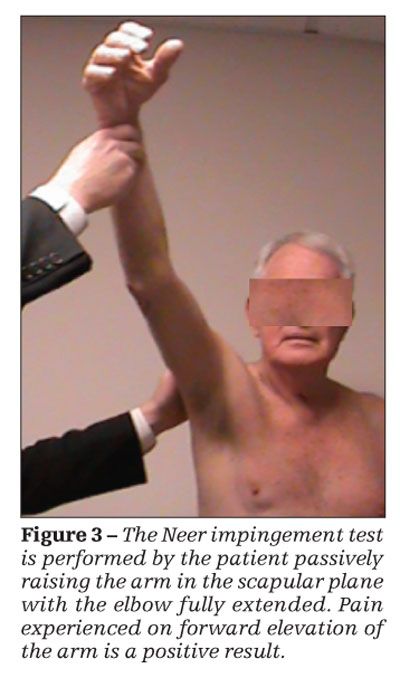
• The Neer impingement test (Figure 3) is performed with the patient's elbow fully extended; the arm is passively raised in the scapular plane (forward elevation). A positive Neer test result is obtained when the patient experiences pain on forward elevation of the arm. The pain classically is eliminated with subacromial injection of lidocaine, although this portion of the test is not typically performed.5
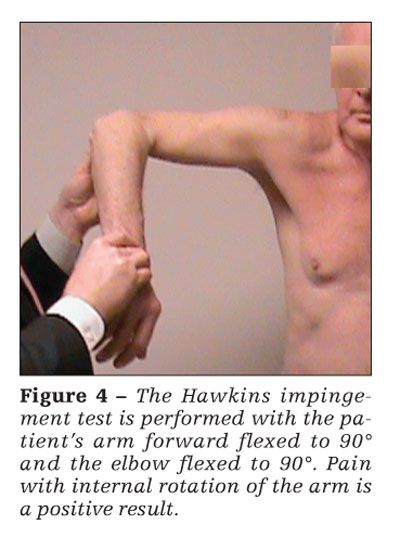
• The Hawkins test (Figure 4) is performed with the patient's arm forward flexed to 90° and elbow flexed to 90°. Pain with internal rotation of the arm signifies a positive Hawkins test result because of impingement of the rotator cuff against the coracoacromial arch.
• The empty can test is performed with the patient's arm internally rotated, pronated, and forward flexed in the scapular plane. Pain or weakness on resistance indicates a supraspinatus tendon
injury.
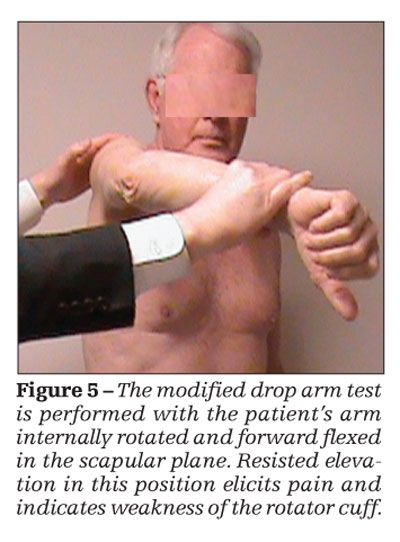
• The drop arm test (Figure 5) is performed with the patient's arm forward flexed to 90°. The patient is then asked to lower his arm slowly to the side. An inability to smoothly control the descent of the arm indicates a supraspinatus tear.
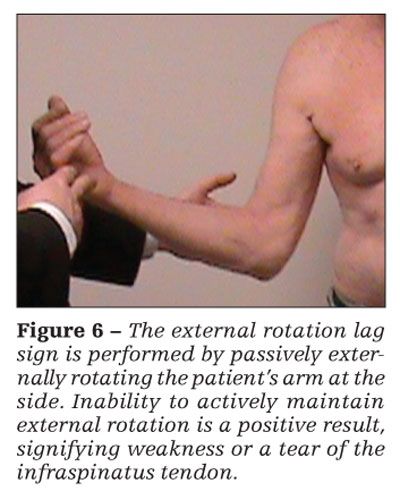
• The external rotation lag sign is performed by passively externally rotating the patient's arm at the side (Figure 6). If the patient cannot maintain this rotation actively, the test result is positive, indicating weakness or a tear of the infraspinatus tendon.
• The hornblower's test is performed by passively abducting and externally rotating the patient's arm. A positive test result is indicated by a patient's inability to actively maintain external rotation, signifying a teres minor injury or tear.
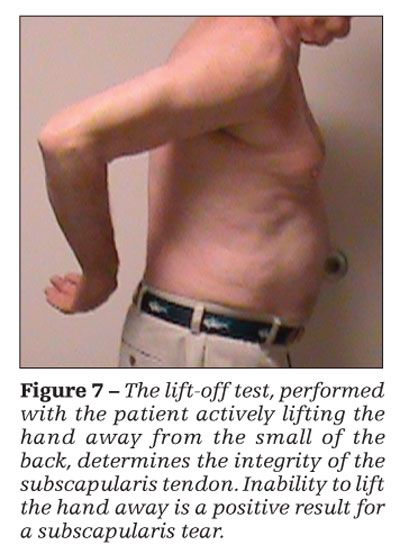
•The lift-off test is performed with the patient's hand against the small of his back (Figure 7). Inability to actively lift the hand off of the back is a positive result; this signifies a tear in the subscapularis tendon.
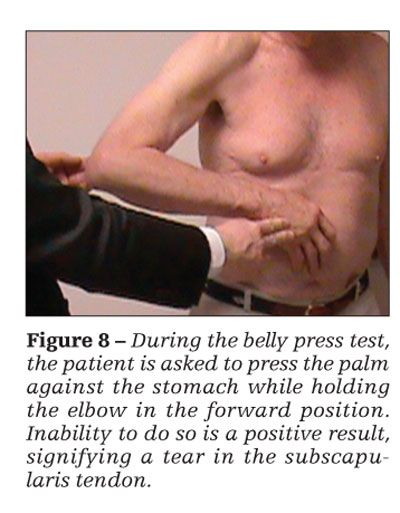
•An alternative to the lift-off test, often performed when there is significant pain or stiffness, is the belly press test (Figure 8). The patient is asked to hold his elbow forward while his hand is pressed against his stomach. Inability to maintain the elbow in the forward position indicates a positive test result, signifying a tear in the subscapularis tendon.
Imaging
Anteroposterior (AP), scapular “Y,” and axillary lateral are the standard radiographic views used to
assess shoulder pain (Figure 9). CT scans may be indicated to determine disease severity in GHOA. Ultrasonography and MRI may be used when soft tissue injury of the rotator cuff, biceps, or labrum is suspected.
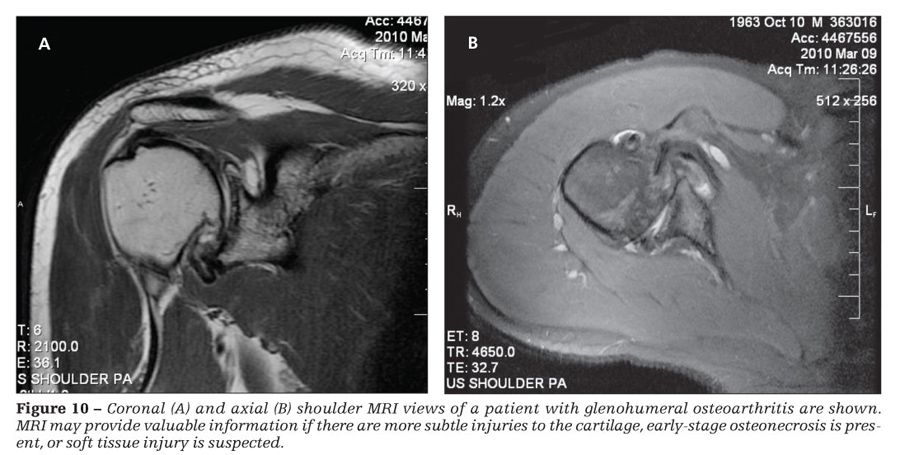
For assessing GHOA, the most informative radiograph is the axillary view, which may reveal joint-space narrowing or the glenoid wear pattern (eccentric or concentric).6 The presence of osteophytes also may be apparent in radiographs (see Figure 9). CT scans may be useful for showing glenoid wear patterns. MRI (Figure 10) may provide valuable information if there are more subtle injuries to the cartilage, early-stage osteonecrosis is present, or soft tissue injury is suspected.
With ACOA, narrowing of the AC joint is evident on the AP x-ray film and osteophyte formation may be visible. With osteolysis of the distal clavicle, erosion of the distal clavicle is seen on the AP radiograph. MRI may be useful for this diagnosis; the result is positive if edema is present on the T2 images on both sides of the AC joint.
Radiographic evaluation of rotator cuff pathology should include supraspinatus outlet, axillary, and AP views in neutral, internal, and external rotation. These views allow for determination of acromion type, the presence of an acromial spur, and the distance between the acromion and the humerus.
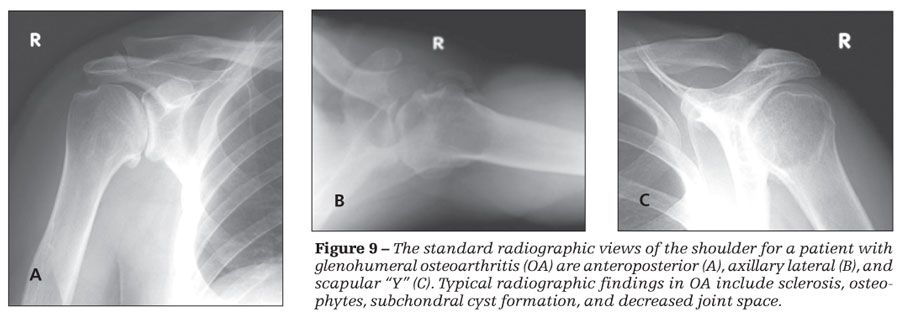
Bigliani and associates7 described 3 types of acromion: 1, “flat”; 2, “curved”; and 3, “hooked.” A large spur in the coracoacromial ligament or a type 2 or type 3 acromion may be seen on scapular lateral x-ray films and is associated with rotator cuff disease or a tear.7 Patients with large rotator cuff tears may have a decreased acromiohumeral interval, which usually is more than 7 mm in patients who do not have a history of shoulder pain.8
Ultrasonography and MRI are useful modalities for assessing rotator cuff tear size and location as well as tissue quality.9 The incidence of partial-thickness rotator cuff tears is higher than was originally thought; therefore, MRI has become a common imaging modality for the rotator cuff. The coronal view is the most useful for assessing the supraspinatus and infraspinatus tendons. Scapular plane images are useful for evaluating muscle atrophy; the axial view is important for evaluating subscapularis and biceps tendon pathology (see Figure 10).9
MRI is particularly useful for assessing osteonecrosis, which may not be seen on plain radiographs. Subchondral edema, necrosis, and collapse of overlying cartilage may be seen on MRI.
When to refer
Referral to an orthopedic surgeon who specializes in the upper extremity should be made when:
• The physician makes a diagnosis of fracture on the basis of shoulder radiographs.
• There is concern about a possible rotator cuff tear.
• Conservative management of the patient's shoulder pain has not been successful.
References:
References
1. Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis. 1998;57:649-655.
2. van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis. 1995;54:959-964.
3. McBeth J, Jones K. Epidemiology of chronic musculoskeletal pain. Best Pract Res Clin Rheumatol. 2007;21:403-425.
4. Ellman H, Harris E, Kay SP. Early degenerative joint disease simulating impingement syndrome: arthroscopic findings. Arthroscopy. 1992;8:482-487.
5. Neer CS 2nd. Impingement lesions. Clin Orthop Relat Res. 1983;173:70-77.
6. Nakagawa Y, Hyakuna K, Otani S, et al. Epidemiologic study of glenohumeral arthritis with plain radiography. J Shoulder Elbow Surg. 1999;8:580-584.
7. Bigliani LU, Morrison DS, April EW. The morphology of the acromion and its relationship to rotator cuff tears. Orthop Trans. 1986;10:216.
8. Neer CS 2nd, Craig EV, Fukuda H. Cuff-tear arthropathy. J Bone Joint Surg. 1983;65A:1232-1244.
9. Tirman PF, Steinbach LS, Belzer JP, Bost FW. A practical approach to imaging of the shoulder with emphasis on MR imaging. Orthop Clin North Am. 1997;28:483-515.




