Article
Mortality Estimates in Elderly Atherosclerosis Patients Improved By Knowledge of Exercise Habits
When asked to elderly patients undergoing coronary artery calcium (CAC) scans, the results of a single question offer providers a better understanding of the individual’s risk of death: "On a scale of 1 - 10, how much do you exercise (0-none, 10-always)?"
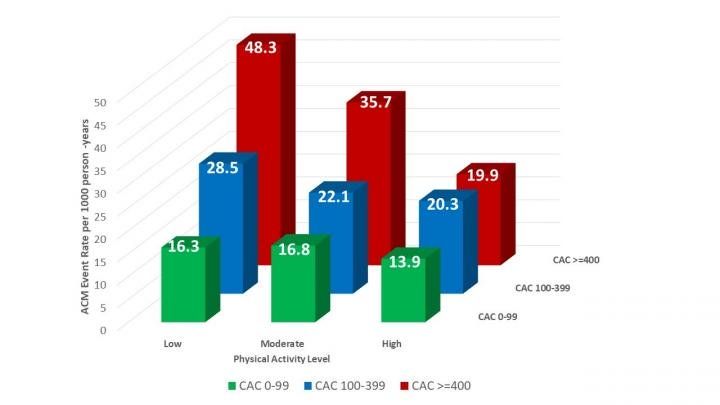
Relationship between self-reported physical activity among seniors >65 years old, the amount of atherosclerotic abnormality on CAC scanning and observed mortality during a mean follow up of 10.6 years. CREDIT: Mayo Clinic Proceedings: Innovations, Quality & Outcomes
When asked to elderly patients undergoing coronary artery calcium (CAC) scans, the results of a single question offer providers a better understanding of the individual’s risk of death: "On a scale of 1 - 10, how much do you exercise (0-none, 10-always)?"
As it turns out, Elderly patients with high levels of atherosclerosis detected by CAC scans, who reported very frequent exercise, had a lower mortality rate than patients who reported getting little or no exercise and a mortality rate similar to patients with low levels of atherosclerosis who exercised rarely or never. In other words, regular exercise overcomes the negative impact of atherosclerotic disease – at least in terms of mortality.
The results of the study were published in Mayo Clinic Proceedings: Innovations, Quality & Outcomes.
"Our study is the first to assess - and show - that this assessment of exercise activity in the elderly strongly influences the risk of death when significant atherosclerosis is detected on CAC scanning," explained lead investigator Alan Rozanski, MD, Professor of Medicine (Cardiology) at the Icahn School of Medicine at Mount Sinai, and Director of Nuclear Cardiology and Cardiac Stress Testing and Chief Academic Officer for the Department of Cardiology at Mount Sinai Morningside, New York, NY, USA.
"A notable aspect was that the use of just a single, self-reported question regarding exercise served to risk stratify older patients if they had elevated coronary artery calcium scores," said Rozanski.
The research examined data from 2,318 patients between the ages of 65 and 84 years who were referred for CAC screening between August 1998 and November 2016, and who died more than one year after the scan. The patients completed a questionnaire at the time of their scan, which asked about chest pain symptoms, cardiac risk factors, medication use, and physical activity. Patients self-reported their physical activity on a scale from 0-none to 10-always. Resting heart rate, blood pressure, height, and weight were recorded. Medical history of dyslipidemia, diabetes, hypertension, and smoking was identified.
The patients were followed for an average of 10.6 years to assess rates of death. During this time, 23 percent had died. For the entire cohort, the annualized mortality rate was 2.3 percent per year, with the highest mortality occurring among patients reporting low physical activity (2.9 percent per year) and the lowest mortality occurring among patients reporting high physical activity (1.7 percent per year).
Among patients with low CAC scores (0-99), survival was similar for each level of physical activity. In contrast, in patients with moderate CAC scores (100-399), the risk for all-cause mortality increased 2.07-fold among patients with low physical activity compared with patients with high physical activity. In patients with CAC scores over 400, all-cause mortality increased 2.35-fold for patients with low versus high activity.
Among all clinical parameters, age and the magnitude of CAC score were the most potent predictors of mortality. Notably, among all other variables, including chest pain symptoms, smoking, and obesity, physical activity was the next most potent predictor.
Dr. Rozanski and colleagues noted that there are several factors that could explain the observations of this study. For example, patients who reported high physical activity had better health profiles, with lower frequency of hypertension, smoking, and diabetes. Of patients reporting high physical activity, only 7.7 percent were obese, while more than 25 percent of patients reporting low physical activity were obese.
"Our results indicate that a simple assessment of self-reported daily-life physical activity can substantially improve the effectiveness of CAC scanning for risk stratifying older adults and is strongly encouraged," said Dr. Rozanski. "This is consistent with recent suggestions to make assessment of physical activity a 'fifth vital sign' that should be entered into patient electronic medical records, along with body temperature, pulse rate, respiration rate, and blood pressure."
"Associations Among Self-reported Physical Activity, Coronary Artery Calcium Scores, and Mortality Risk in Older Adults," by Alan Rozanski, MD; Yoav Arnson, MD; Heidi Gransar, MS; Sean W. Hayes, MD; John D. Friedman, MD; Louise E.J. Thomson, MBChB; Damini Dey, PhD; and Daniel S. Berman, MD (https://doi.org/10.1016/j.mayocpiqo.2020.02.005). It appears in Mayo Clinic Proceedings: Innovations, Quality & Outcomes volume 4, issue 3 (June 2020) published by Elsevier. It is openly available.

FDA Approves Crinecerfont for Congenital Adrenal Hyperplasia



