Article
MRI for Evaluating Knee Pain in Older Patients: How Useful Is It?
Knee pain is a common complaint in older patients, andosteoarthritis is the leading cause.We prospectively evaluated the diagnosticpatterns of nonorthopedic physicians in 100 consecutive patientsolder than 60 years who had knee pain. Our study shows thatthere is a lack of consensus about the use radiographic studies for diagnosisof knee pain in older patients.Weight-bearing radiographs areideal for evaluating knee pain. MRI frequently is overly sensitive in detectingpathology and often underestimates joint-space narrowingand arthrosis. MRI also represents a much larger cost and burden onthe health care system. MRI is indicated when the cause of knee painis not readily apparent after careful physical and radiographic evaluation.(J Musculoskel Med. 2008;25:500-504)
ABSTRACT: Knee pain is a common complaint in older patients, and osteoarthritis is the leading cause. We prospectively evaluated the diagnostic patterns of nonorthopedic physicians in 100 consecutive patients older than 60 years who had knee pain. Our study shows that there is a lack of consensus about the use radiographic studies for diagnosis of knee pain in older patients. Weight-bearing radiographs are ideal for evaluating knee pain. MRI frequently is overly sensitive in detecting pathology and often underestimates joint-space narrowing and arthrosis. MRI also represents a much larger cost and burden on the health care system. MRI is indicated when the cause of knee pain is not readily apparent after careful physical and radiographic evaluation. (J Musculoskel Med. 2008;25:500-504)
Knee pain is one of the most common musculoskeletal complaints in patients older than 50 years.1-3 Up to 30% of these patients report persistent knee pain lasting more than 3 months.1 As the population ages and patients continue to be active, the proportion of patients with knee symptoms and pathology probably will increase. Although osteoarthritis (OA) overwhelmingly is the most common cause of knee pain in this patient population, "acute on chronic" events (eg, degenerative meniscal tears and ligament injuries) may add to patients' pain and disability.
The ease, availability, and sensitivity of MRI as an initial diagnostic tool create a misconception that this is the test of choice for patients presenting with knee pain. In our opinion, there is a tendency to overuse expensive and often unnecessary imaging of older patients with knee pain, resulting in delays in diagnosis and treatment, inconveniences to patients, and increased health care costs.
In this article, we present findings from our study that evaluated the diagnostic patterns of nonorthopedic physicians in the evaluation and treatment of older patients with knee pain. We also offer a diagnostic and radiographic algorithm.
MATERIALS AND METHODS
We prospectively evaluated the diagnostic patterns of nonorthopedic physicians in 100 consecutive patients older than 60 years who had knee pain. There were 68 women and 32 men (mean age, 78 years; range, 60 to 99 years). Demographic information recorded for each patient included referring physician specialty, types of radiographic studies, and dates. A group of board-certified orthopedic surgeons who had a subspecialty in hip and knee reconstruction examined all patients. The diagnosis, treatment, outcome, and any required additional testing were recorded.
RESULTS
The radiographic studies available for each patient at the time of initial evaluation are outlined in Figure 1. Of the 100 new patients, 13 presented to the office with no x-ray films, 26 had had only MRI scans of their knees, 22 had been evaluated with both MRI scans and x-ray films, and 29 presented with non–weight-bearing radiographs of their knees; 32 patients in this series had been evaluated previously with standing anteroposterior (AP) and lateral x-ray films of their knees.
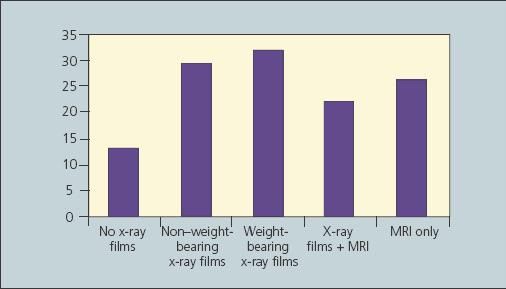
Figure 1 –
This graph shows the radiographic studies available for each patient with knee pain at the time of initial evaluation in the authors' prospective study of the diagnostic patterns of nonorthopedic physicians in 100 consecutive patients older than 60 years.
Of the 22 patients who already had had an MRI scan and plain radiographs of their knees, 8 had an MRI scan before knee x-ray films; 6 patients had obtained both the MRI scan and the x-ray films on the same day. Only 8 patients had been evaluated with plain radiographs before MRI evaluation.
The most common diagnosis in this group of patients was OA (n = 93), followed by referred pain from the hip or low back (n = 2), osteonecrosis (n = 1), osteochondral defect (n = 1), loose body (n = 1), knee contusion (n = 1), and chondrocalcinosis (n = 1) (Figure 2). Of the patients who previously had been evaluated with MRI, 36 had evidence of meniscal tears on MRI but only 1 tear was thought to be clinically significant to warrant arthroscopic meniscectomy and debridement.
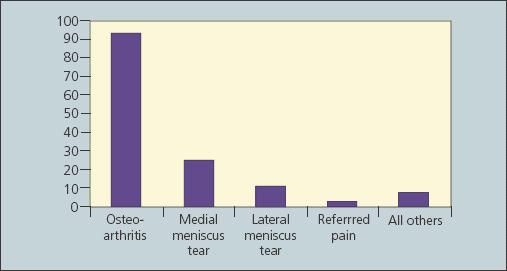
Figure 2 –
The diagnoses made with the available imaging on patient presentation to the orthopedist in the study are shown here. Osteoarthritis is overwhelmingly the primary cause of knee pain in this age population.
In terms of disposition, 54 patients were treated conservatively with rest, activity modification, and anti-inflammatory medications (Figure 3). These patients also were given injections of either cortisone or viscosupplementation and were referred for physical therapy evaluation and treatment. Thirty-four patients had significant evidence of OA on plain radiographs; they were counseled and subsequently underwent total knee arthroplasty. Only 1 patient who was evaluated was referred for knee MRI. Overall, 46 patients had no studies (n = 13) or had inadequate studies that required additional studies, leading to delays in diagnosis and management of their knee symptoms.
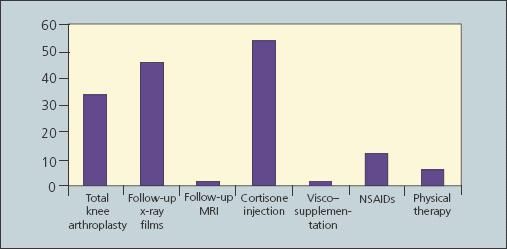
Figure 3 –
The interventions for knee pain chosen at the initial orthopedic visit in the study are shown in this graph.
The breakdown of imaging studies ordered for patients referred by physicians in specialties rather than primary care was quite similar to that for other patients in this study. Two patients presented with no initial studies, 4 patients presented with non–weight-bearing x-ray films of the knee, 3 patients presented with only an MRI scan, and 1 patient had been evaluated previously with both plain x-ray films and MRI. Of note, 2 patients who were referred by nonsurgical sports medicine physicians presented to our clinic with only an MRI scan of their knees, but they had such severe degenerative joint disease that they were counseled and subsequently treated with knee replacement surgery.
DISCUSSION
Lack of consensus
Our study shows that among nonorthopedic physicians there is a lack of consensus about the use of radiographic studies for diagnosis of knee pain in older patients. In those patients 60 years and older, OA is the most common cause of knee pain. Studies have shown that almost 50% of persons older than 55 years have radiographic changes consistent with arthritis and that the number increases to more than 75% in patients older than 65 years.4,5 Although current technologies allow for obtaining detailed imaging of bone, ligament, and cartilage about the knee, they do not replace a detailed history and careful physical examination.
Musculoskeletal medicine de-emphasized
Because of a scarcity of time and a lack of resources, musculoskeletal medicine has been de-emphasized in medical school and residency curricula. As a result, primary care physicians are not universally comfortable with the workup and examination of musculoskeletal complaints.
In a recent study of 122 medical schools, only 41.8% had preclinical instruction as part of their basic science curriculum and only 20.5% required their students to complete a clerkship in musculoskeletal medicine.6 In another study, 82% of 85 recent medical school graduates failed to obtain at least a grade of 73% on a basic musculoskeletal medicine competency examination validated by 124 orthopedic program directors.7 In addition, in a recent survey of 5487 second-year primary care residents, a large percentage expressed a lack of confidence in evaluating musculoskeletal complaints.8 Therefore, we are concerned that the lack of training in musculoskeletal medicine translates into potentially inappropriate use of radiographic modalities in the evaluation of patients with knee pain.
Ideal for knee pain evaluation
Standing (weight-bearing) radiographs of the knee are ideal for evaluating knee pain (Figure 4). In addition to identifying potentially dangerous conditions,such as fractures and malignancy, knee radiographs (standing AP, lateral, and Merchant views) allow the clinician to assess joint-space narrowing in all 3 compartments.

MRI often is overly sensitive in detecting pathology (eg, meniscal tears) and often underestimates the joint-space narrowing and arthrosis in this patient population (Figure 5). MRI studies have reported a prevalence of greater than 50% of meniscal lesions in asymptomatic patients older than 50 years.9-11
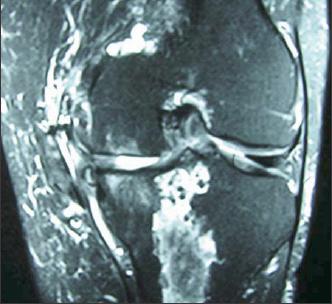
Figure 5 –
The MRI scan obtained for the 64-year-old man with knee pain shows a medical meniscal tear with signs of medial osteoarthritis. Like the non–weight-bearing x-ray films, it was not needed for determining the patient's best pain relief option.
In addition, MRI represents a much larger cost and burden on the health care system. In the Philadelphia area, the Medicare reimbursement for plain radiographs of the knee is a technical fee of $25.33 and a professional fee of $10.37; the reimbursement for an MRI evaluation is a technical fee of $478.67 and a professional fee of $72.12. Consequently, plain 3-view weight-bearing x-ray films of the knee provide a higher initial diagnostic yield than MRI and are more cost effective in the evaluation of patients with knee pain.
Arthroscopy warranted?
In our study, 48 patients presented at their initial evaluation having had an MRI scan of their knees. Although the majority of these patients (75%) had MRI evidence of meniscal tears, OA of the knee was the main cause of their knee pain and only 1 patient warranted arthroscopic meniscectomy. In fact, 16 of these patients had such severe arthritic changes on plain radiographs that they subsequently underwent knee replacement surgery.
In addition, there is little evidence that arthroscopy in patients with coexistent knee OA and meniscal tears can reliably provide durable pain relief and prevent the need for subsequent joint replacement. In a cross-sectional cohort study of patients with OA of the knee managed with arthroscopic debridement, Aaron and coworkers12 reported significant relief in only 25% of the patients. Similarly, in a double-blind prospective study that compared arthroscopy with placebo, Moseley and colleagues13 found no difference between the 2 groups in terms of pain relief and satisfaction. Although these studies have weaknesses, it is clear that arthroscopic debridement in patients with coexistent arthritis and meniscal tears is more predictable at relieving mechanical symptoms (eg, catching and locking) than at relieving knee pain.
Evaluation algorithm
To our knowledge, currently there is no algorithm set for evaluation of chronic knee pain in patients older than 60 years. In patients with acute knee trauma or pain, radiographs should be obtained if the patient is unable to bear weight or to flex the knee more than 90° or if there is tenderness in the patella or the fibular head. Following this algorithm, Jenny and coworkers14 reported 100% sensitivity for identifying fractures and prevented up to 50% of unnecessary radiographs.
In contrast, if knee pain persists past the initial injury or the patient can bear weight on the extremity, weight-bearing radiographs can provide much more valuable information and should be the screening tool of choice.There is no need for emergent MRI evaluation before the use of plain x-ray films in this age category.
MRI is indicated when the cause of knee pain is not readily apparent after careful physical and radiographic evaluation. If plain x-ray films do not reveal significant jointspace narrowing, MRI may be indicated to rule out stress fractures, meniscal pathology, malignancies, and other conditions. Symptomatic meniscal tears should be suspected in patients complaining of persistent knee effusions and mechanical symptoms,such as catching or locking of the knee.
CONCLUSION
Weight-bearing radiographs of the knee are the screening tests of choice in the evaluation of patients older than 60 years with knee pain. Because there is a high prevalence of asymptomatic degenerative meniscal tears in patients older than 60 years, the presence of a positive MRI result rarely alters initial management.MRI evaluation is indicated only in patients who have persistent knee pain with normal standing x-ray film results and after a thorough physical examination of the knee.
References:
References
- 1. Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis. 2001;60:91-97.
- 2. Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778-799.
- 3. Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights, part 1: the disease and its risk factors. Ann Intern Med. 2000;133:635-646.
- 4. Gresham GE, Rathey UK. Osteoarthritis in knees of aged persons: relationship between roentgenographic and clinical manifestations. JAMA. 1975;233:168-170.
- 5. Claessens AA, Schouten JS, van den Ouweland FA, Valkenburg HA. Do clinical findings associate with radiographic osteoarthritis of the knee? Ann Rheum Dis. 1990;49:771-774.
- 6. DiCaprio MR, Covey A, Bernstein J. Curricular requirements for musculoskeletal medicine in American medical schools.
J Bone Joint Surg. 2003;85A:565-567.
- 7. Freedman KB, Bernstein J. Educational deficiencies in musculoskeletal medicine. J Bone Joint Surg. 2002;84A: 604-608.
- 8. Clawson DK, Jackson DW, Ostergaard DJ. It’s past time to reform the musculoskeletal curriculum. Acad Med. 2001;76:709-710.
- 9. Cicuttini F, Ding C, Wluka A, et al. Association of cartilage defects with loss of knee cartilage in healthy, middle- age adults: a prospective study. Arthritis Rheum. 2005;52:2033-2039.
- 10. Kaplan LD, Schurhoff MR, Selesnick H, et al. Magnetic resonance imaging of the knee in asymptomatic professional basketball players. Arthroscopy. 2005;21:557-561.
- 11. Beattie KA, Boulos P, Pui M, et al. Abnormalities identified in the knees of asymptomatic volunteers using peripheral magnetic resonance imaging. Osteoarthritis Cartilage. 2005;13:181-186.
- 12. Aaron RK, Skolnick AH, Reinert SE, Ciombor DM. Arthroscopic debridement for osteoarthritis of the knee. J Bone Joint Surg. 2006;88A:936-943.
- 13. Moseley JB, O’Malley K, Petersen NJ, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81-88.
- 14. Jenny JY, Boeri C, El Amrani H, et al. Should plain x-rays be routinely performed after blunt knee trauma? A prospective analysis. J Trauma. 2005;58:1179-1182.




