Article
Multicomponent Intervention Program may Improve QoL in Patients with Fibromyalgia
Author(s):
Investigators note that healthcare approaches may benefit from including patient-reported experiences of living with and being treated for fibromyalgia.
A multicomponent intervention (MCI) program, combining health education, cognitive behavioral therapy (CBT), and physical activity was conducted for patients with fibromyalgia syndrome (FMS) in an attempt to improve symptom self-management and quality of life (QoL). Results indicated that the patients regarded the program as an insightful experience that encouraged acceptance and illness knowledge, along with improving coping skills and QoL, according to a study published in Environmental Research and Public Health.1
“Existing research indicates that poor perception of illness, including perceiving a fluctuating and unpredictable illness course and a low emotional representation of FMS, which means not connecting emotionally with one’s health condition, is associated with higher medical costs,” investigators explained. “Therefore, healthcare approaches may benefit from including patients’ subjective experiences of living with and being treated for FMS.”
A qualitative interview study was performed in primary care centers in South Catalonia, Spain, to understand patients’ lived experiences throughout the intervention. The MCI program included a 12-week/2-hour session interdisciplinary program, along with usual clinical care (UCC). Topics covered included the pharmacology and neurophysiology of pain, nutrition, insomnia management, postural hygiene, memory, sexuality, stretching, coordination exercises and pain, breathing and relaxation techniques, attention, and emotional management. Participants were urged to practice what they learned during the MCI. Eligible participants were adults, had a clinical diagnosis of FMS, and had oral and writing skills in Spanish and/or Catalan.
A total of 10 female patients, with a mean age of 58.5 years, were interviewed via either phone calls or face-to-face, with prior signed inform consent, which were recorded and analyzed. Topics covered included an introduction, overall opinion about the MCI, possible benefits, implementation of coping strategies, changes regarding psychological and emotional changes, social feedback, aspects of the program that may be improved, and additional comments and suggestions.
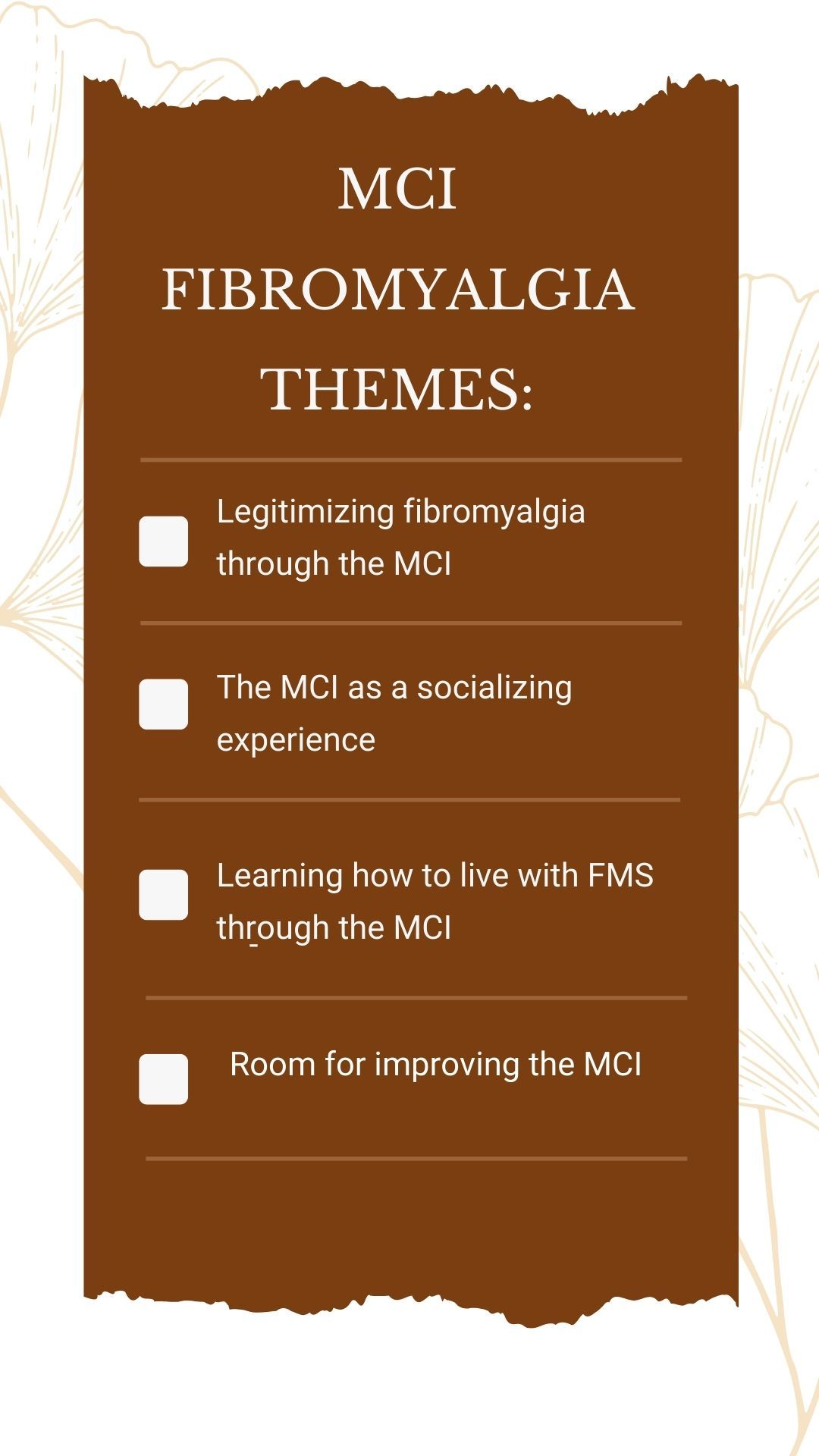
The 4 themes that emerged were legitimizing fibromyalgia through the MCI, the MCI as a socializing experience, learning how to live with FMS via the MCI, and any room for improvement within the MCI. Study participants agreed that the program was an insightful experience that promoted illness knowledge and acceptance and improved patients’ coping skill and self-management of symptoms. Including additional psychological guidance, teaching relatives about FMS, and group therapy were proposed ideas for enhancing the program.
Recruitment was systematically and purposively conducted to ensure variability and avoid selection bias. Efforts were made to collect quality data and rigorously evaluate it, thus allowing investigators to understand the impact and benefits of an MCI program on patients’ subjectivity. Limitations included the small, exclusively female sample of patients. However, FMS is much more prevalent in women when compared with men. Benefits of the program may have been overestimated as interviewees included in the study had high assistance records and a willingness to participate in the study. Investigators note that results may not be generalizable beyond the study sample.
“Our findings have contributed to gaining insight into the subjective impact of the MCI and identifying new therapeutic targets to tailor the program to patients’ needs, which will hopefully increase its effectiveness and improve their quality of life,” investigators concluded.
Reference:
Arfuch VM, Caballol Angelats R, Aguilar Martín C, et al. Patients' Lived Experience in a Multicomponent Intervention for Fibromyalgia Syndrome in Primary Care: A Qualitative Interview Study. Int J Environ Res Public Health. 2022;19(20):13322. Published 2022 Oct 15. doi:10.3390/ijerph192013322




