Article
Neither Linagliptin nor Glimepiride Increases Cardiovascular Risk in Diabetes
Author(s):
Adults with early type two diabetes and elevated cardiovascular risk may be able to safely take linagliptin or sulfonylurea (glimepiride) without increasing their risk of cardiovascular events, researchers report in JAMA.
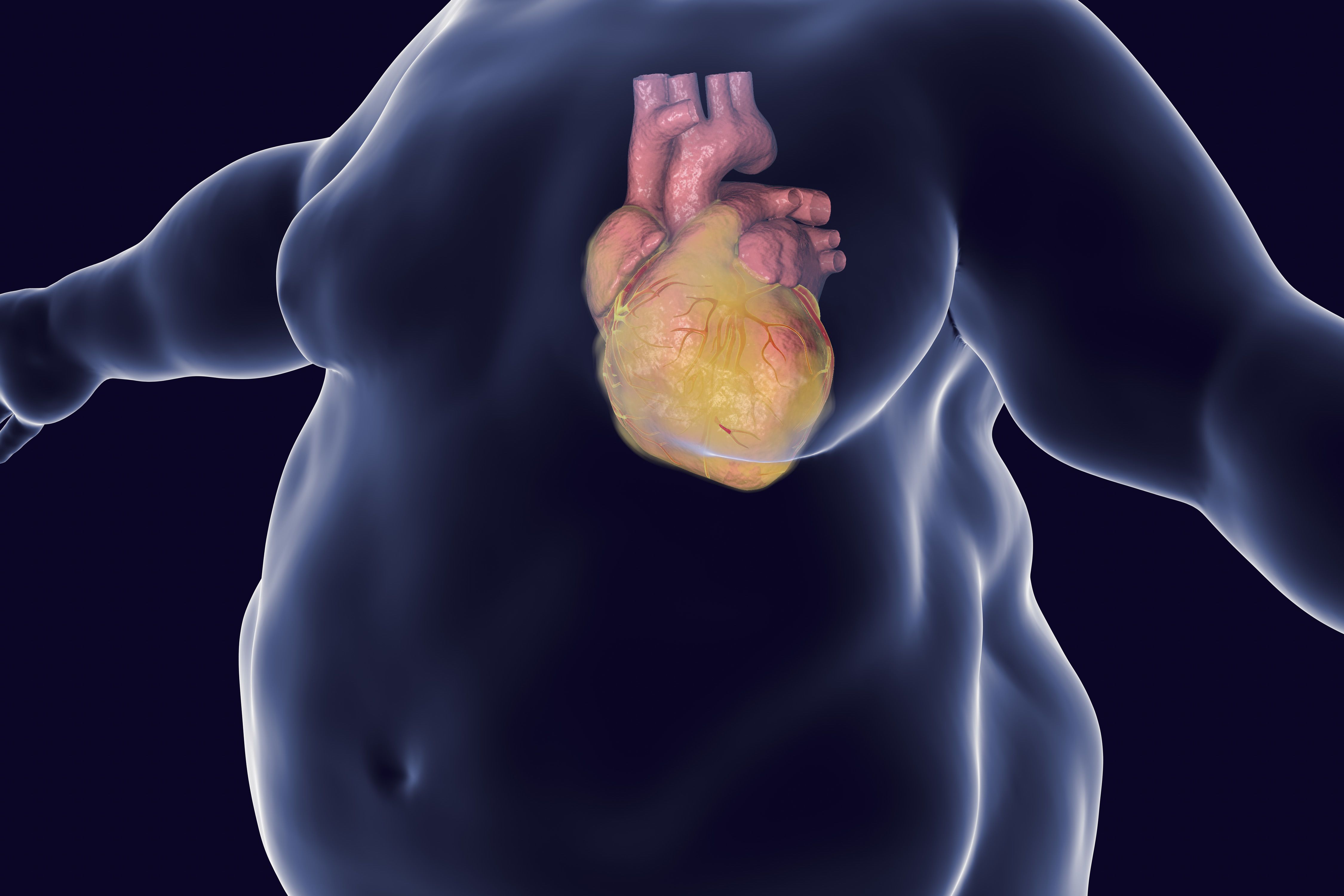
Adults with early type two diabetes and elevated cardiovascular risk may be able to safely take linagliptin or sulfonylurea (glimepiride) without increasing their risk of cardiovascular events, researchers report in JAMA. (©Kateryna_Kon,AdobeStock_185028145)
Adults with early type two diabetes and elevated cardiovascular risk may be able to safely take linagliptin or sulfonylurea (glimepiride) without increasing their risk of cardiovascular events, researchers report in JAMA.
Linagliptin is a dipeptidyl peptidase-4 (DPP-4) inhibitor that, like glimepiride, is a widely used second-line glucose-lowering agents. Researchers, who were led by Nikolaus Marx, M.D., of University Hospital Aachen in Germany, conducted a randomized noninferiority clinical trial of 6,033 participants (mean age 64 years, 40 percent women) who were followed for slightly more than six years. They had hemoglobin A1c levels of 6.5 to 8.5 percent and had atherosclerotic cardiovascular disease with other cardiovascular risk factors.
"The current study demonstrates noninferior cardiovascular safety effects for linagliptin vs glimepiride when used predominantly as a second-line glucose-lowering treatment option after metformin," the authors wrote.
Participants were randomized to receive 5 mg daily daily of linagliptin or 1-4 mg daily of glimepiride in addition to standard care, including metformin and other glucose-lowering agents as needed.
In a median follow-up time of 6.3 years in both groups, the primary outcome, which was the time to first occurrence of cardiovascular death, non-fatal myocardial infarction, or nonfatal stroke, occurred in 11.8 percent of those given linagliptin versus 12 percent of the glimepiride group, a nonsignificant difference with hazard ratio 0.98 and P less than 0.001 for non-inferiority.
Hypoglycemia was more common with glimepiride, with rates of moderate or severe hypoglycemic events occurring in 8.4 versus 1.4 per 100 participant years (hazard ratio 0.18, P less than 0.001).
The findings with this trial, called Cardiovascular Outcome Study of Linagliptin vs Glimepiride in Type 2 Diabetes (CAROLINA), could help alleviate a long-held concern about cardiovascular safety of the sulfonylurea class, which dates back to a 50-year-old study conducted with an older-generation sulfonylurea agent. CAROLINA is the first head-to-head trial comparing long-term effects of the two drug classes on cardiovascular morbidity and mortality in type two diabetes.
Neither drug provides a cardiovascular advantage, as do some of the sodium glucose cotransporter-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1)-receptor agonists.
In an accompanying editorial, Deborah J.Wexler, M.D., of Massachusetts General Hospital in Boston, wrote that the findings suggest “clinicians can continue to use low-cost sulfonylurea (glimepiride) added to metformin for management of hyperglycemia in type 2 diabetes with confidence in their effectiveness for reduction of microvascular complications as well as their cardiovascular safety. The adverse effect profile of sulfonylurea (glimepiride) and their very low cost must be balanced against characteristics of other glucose-lowering medications as clinicians consider the best approach for an individual patient.”
Dr. Wexler stated that further evidence on the comparative effectiveness of glimepiride and a DPP-4 inhibitor, a GLP-1 receptor agonist, and basal insulin, each added to metformin, is expected with the publication of her group’s Glycemia Reduction Approaches in Diabetes: A Comparative Effectiveness (GRADE) Study, in 2022.
The authors of the study state that because linagliptin is associated with less weight gain and hypoglycemia than glimepiride, it is the preferred drug of the two to add when metformin alone isn’t sufficient to achieve hemoglobin A1c targets. On the other hand, the sulfonylurea (glimepiride) is much less expensive.
These findings were first presented at the American Diabetes Association (ADA) 79th Scientific Sessions in June and again at the annual meeting of the European Association for the Study of Diabetes on September 16.
REFERENCE
Julio Rosenstock, MD; Steven E. Kahn, MB, ChB; Odd Erik Johansen, MD, PhD; et al. “Effect of Linagliptin vs Glimepiride on Major Adverse Cardiovascular Outcomes in Patients With Type 2 Diabetes: The CAROLINA Randomized Clinical Trial.” JAMA. doi:10.1001/jama.2019.13772 Published online September 19, 2019.




