Article
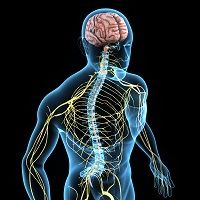
New Expression Found Responsible for Neuropathic Pain
Author(s):
While it was recently determined that endoplasmic reticulum stress (ER) plays an intricate role in neuropathic pain, a team from Hiroshima University has found another factor that contributes to pain.
While it was recently determined that endoplasmic reticulum stress (ER) plays an intricate role in neuropathic pain, a team from Hiroshima University has found another factor that contributes to pain.
Neuropathic pain after a peripheral nerve injury is due in part to the downregulation of spinal astrocyte connexin43 (Cx43) expression, according to a study published in Brain, Behavior, and Immunity. Even though there are several types of Cx in the spinal cord, Cx43 is associated with neuroinflammation (such as that observed in multiple sclerosis) and other neurological disorders, which led the team to explore the role of Cx43 expression in pain.
“The inflammatory cytokinetumor necrosis factor (TNF) mediates the downregulation of Cx43 expression, which leads to decreased expression of the glutamate transporter GLT-1 and enhanced glutamatergic neurotransmission,” a news release explained.
Using mice, the researchers found that spinal cord inflammation following peripheral nerve injury caused the release of TNF and other cytokines. When this happens, downregulation of Cx43 and GLT-1 kicks in, which increases excitatory synaptic activity.
“The source of this dysfunctional glutamatergic neurotransmission is likely decreased clearance of glutamate from the synapse rather than increased glutamate release into the synapse,” the team verified.
However, the researchers were able to reverse the hypersensitivity by restoring the Cx43 expression with adenovirus vector. This suggests the importance of the specific spinal astrocyte in neuropathic pain.
“In addition, downregulated GLT-1 was reversed by restoration of Cx43 by adenovirus vector expressing Cx43. It is possible that Cx43 directly regulates GLT-1 expression and function,” said one of the authors Norimitsu Morioka, an associate professor of applied life sciences at the university, in the statement.
These findings could provide a target for the development of new pharmaceutical treatments, yet more research is needed to further the understanding.





