Article
No Need to Routinely Screen Osteoporosis Patients for Celiac Disease
Author(s):
Contrary to current guideline recommendations, a new review argues against routine coeliac disease screening for osteoporosis patients.
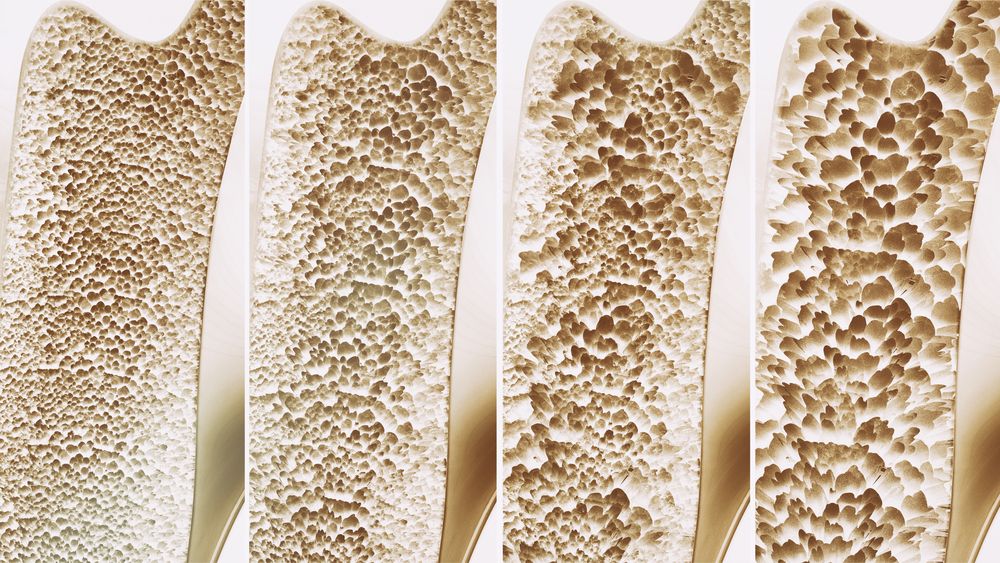
©Crevis/Shutterstock.com
The prevalence of coeliac disease in osteoporosis patients is similar to that of the general population, according to a new systematic review in Alimentary Pharmacology & Therapeutics.
This finding argues against routinely screening osteoporosis patients for coeliac disease, contrary with current guideline recommendations.
Guidelines published by the British National Institute for Health and Care Excellence in 2015 on the management of coeliac disease recommend assessment of bone mineral density (BMD) at the time of annual physical examination, using the World Health Organization fracture risk assessment tool before considering the need for a dual-energy X-ray absorptiometry (DXA) scan. There is controversy around the validity of fracture risk assessment tools vs DXA in this specific population.
A recent meta-analysis reported that coeliac disease patients are at a 30% increased risk of any fracture and at a 69% increased risk of hip fracture. Another recent meta-analysis found that coeliac disease patients had an increased risk of osteoporosis, and so did a large screening study.
“These studies did not, however, examine the risk of coeliac disease in patients first diagnosed with osteoporosis. Such information is crucial for clinicians as this will guide whether they should screen individuals with osteoporosis for coeliac disease,” stated researchers led by Monika Laszkowska, MD, of the Columbia University College of Physicians and Surgeons in New York, New York. They note that the reported prevalence of coeliac disease in those with osteoporosis has varied between 0% and 33%.
Laszkowska and colleagues conducted a systematic review of articles published in PubMed, Medline, or EMBASE through May 2017 to identify studies looking at prevalence of coeliac disease in patients with osteoporosis. They identified 8 relevant studies, comprising data from 3188 individuals with osteoporosis. Of these, 59 individuals (1.9%) had coeliac disease.
A weighted pooled analysis demonstrated biopsy-confirmed coeliac disease in 1.6% of those with osteoporosis. The heterogeneity was moderate and influenced by the underlying coeliac disease prevalence in the general population. After adding 4 studies, including 814 patients with coeliac disease defined as positive tissue transglutaminase or endomysial antibodies, the pooled prevalence was comparable (1.6%).
“Importantly, the prevalence of coeliac disease did not change when we included studies based on positive coeliac disease serology – the absolute proportion went from 1.9% to 2.6% but the pooled weighted prevalence remained at 1.6%,” wrote the researchers.
Various studies have shown that treatment with a gluten-free diet improved BMD in patients with coeliac disease. “Such studies suggest that treatment of coeliac disease is likely to decrease the excess fracture risk, and therefore a diagnosis of coeliac disease is probably beneficial to individuals with a history of fractures,” wrote the researchers.
The mechanism for osteoporosis in coeliac disease patients likely is multifactorial. “Individuals with coeliac disease often have a low bone density at diagnosis, even in the absence of other symptoms or manifestations of coeliac disease,” they wrote. The researchers suggest this may be due to malabsorption of vitamin D and calcium resulting in secondary hyperparathyroidism, as well as other factors, including chronic inflammation with increased cytokine levels that interfere with bone growth and autoimmune factors.





