Article
Nurse Practitioner Q&A: Screen Risk Factors for Blood Clot Disorder
Author(s):
Blood clots can cause critical or lethal problems in patients, and individuals with antiphospholipid syndrome can experience these events at any location in their bodies. However, there’s not a great deal of clarity on which risk factors are most significant for this condition. In this Q&A, we feature a conversation with Eileen J. Lydon, ANP-BC, a rheumatology nurse practitioner at New York University Langone Orthopedic Hospital, who recently spoke on recommendations for treating patients with antiphospholipid syndrome.
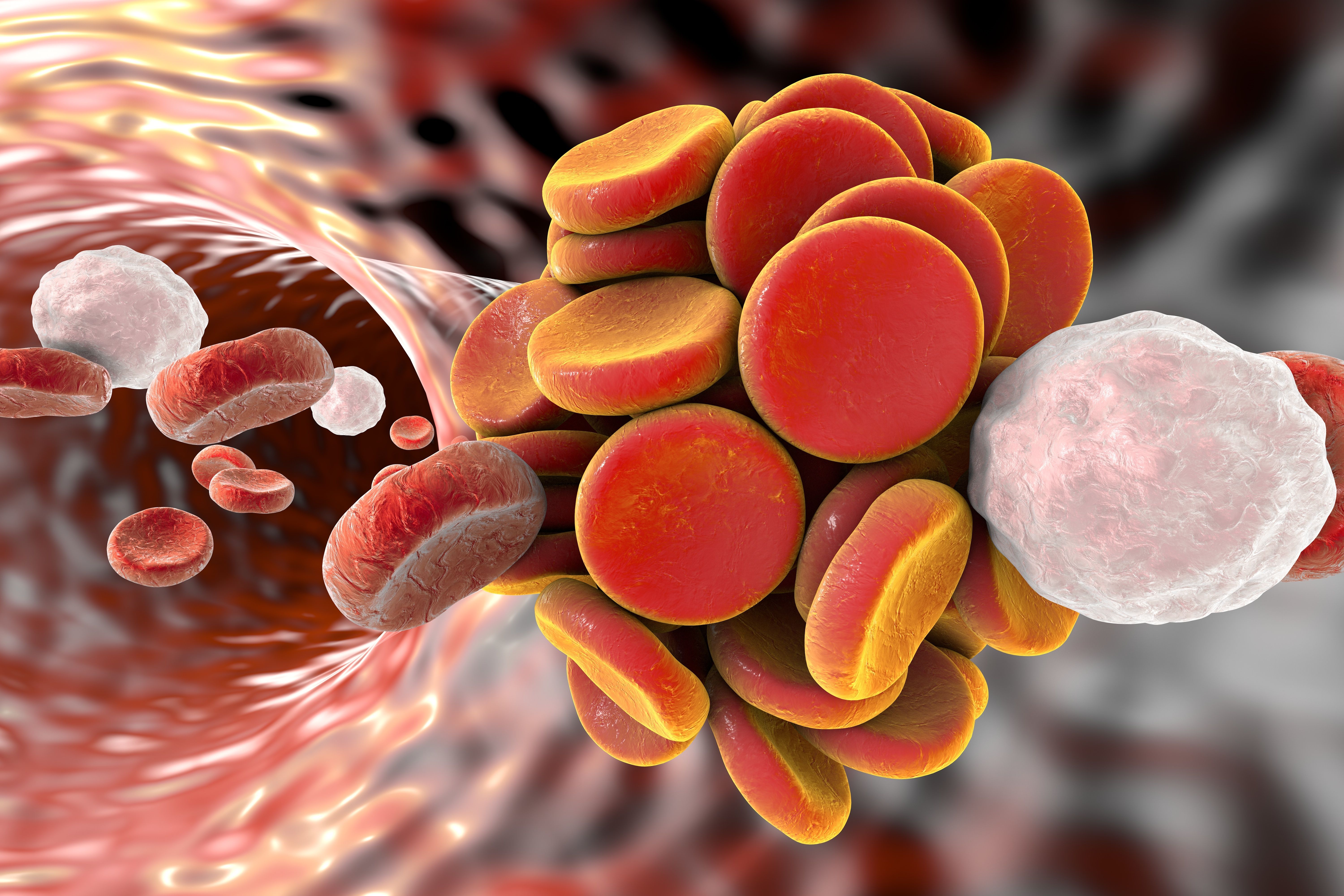
Thromboembol in blood vessel. (©Kateryna_Kon,AdobeStock.com)
Eileen J. Lydon, ANP-BC

Blood clots can cause critical or lethal problems in patients, and individuals with antiphospholipid syndrome can experience these events at any location in their bodies. However, there’s not a great deal of clarity on which risk factors are most significant for this condition.
Fortunately, recent recommendations have shed light on how to best treat patients with antiphospholipid syndrome. In a presentation given at the Rheumatology Nurses Society this summer, Eileen J. Lydon, ANP-BC, a rheumatology nurse practitioner at New York University Langone Orthopedic Hospital, discussed the importance of the nurse’s role in providing care to these patients.
In this Q&A, Ms. Lydon touched on the main points of her presentation.
Q: Within the context of treating rheumatology patients, why is paying attention to antiphospholipid syndrome important, and what role can nurses play?
“It’s an autoimmune disorder that can cause thrombus in the veins or the arteries. It can cause early or late pregnancy losses and premature loss, as well. It’s mostly important because 40 percent of patients who have lupus carry the antibodies for it and can develop antiphospholipid syndrome. Sometimes, we don’t know why certain people clot. But, certainly people with cardiolipin antibodies, who have thromboprophylaxis risk factors, such as hyperlipidemia, high blood pressure, obesity, or women who take oral contraceptives with estrogen, have a higher likelihood. Taking care of these conditions, educating patients about it, making sure they’re properly monitored - these are things the rheumatology nurse population can help with.
Additionally, nurses should always talk with patients about warfarin, a common medication that is used to treat antiphospholipid syndrome. It requires a frequent blood test monitoring and requires that patients stay adherent on the medication, as well. Otherwise, it could be detrimental and deadly. Nurses should always talk with the patient about adherence so they understand the importance of staying on the medication.”
Q: What makes identifying antiphospholipid syndrome tricky?
“Antiphospholipid syndrome can affect any vessel in the body, and that’s important to internalize. Remember what can happen most commonly – the deep vein thrombosis that presents as a painful, swollen calf , a stroke, or recurrent miscarriages after 10 weeks gestation - but, be aware that symptoms and warning signs can pop up anywhere on the body. Also, patients can have non-thrombotic type manifestations, such as valvular heart disease, livedo reticularis or thrombocytopenia, as well as positive non-criteria lab tests.
We also need to be selective in who we test because up to 5 percent of the healthy population have antibodies. People who have lupus, or those less than 50 years of age with an unprovoked thrombosis, or thrombosis that occurs at unusual sites are examples of those who should be tested. In addition, cardiolipin antibodies should be tested once and, then, again after 3 months to avoid over diagnosis, because sometimes they are transiently positive.
Q: Given that diagnosis is complex, is there any clarity on treatment?
“Fortunately, there are new guidelines from EULAR published just a few months ago to help with treatment because there’s been a lot of debate about how to handle antiphospholipid syndrome. One important recommendation is to give low-dose aspirin in those with anticardiolipins who have a high-risk profile, but never had a thrombotic event to help prevent a first event. A high-risk antiphospholipid profile includes a lupus anticoagulant, double or triple positivity or persistently high antiphospholipid titers by the antiphospholipid and global antiphospholipid syndrome score.
Q: What do rheumatologists and rheumatology nurses need to do to ensure they’re maximizing treatment for their patients?
There were three overarching principles discussed in the recent EULAR recommendations that should be part of our practice to reduce thrombotic risk. First, providers need to identify those patients with high-risk profiles, autoimmune disease, especially lupus, presence of cardiovascular disease, as well as those who had a history of thrombotic or obstetric events in the past.
Second, screen and manage cardiovascular and venous thrombosis risk factors. Also, use low molecular weight heparin in high-risk situations, such as surgery, prolonged immobilization, and post partum.
Finally, educate and counsel all patients treated with warfarin on the importance of adherence and the need for close INR monitoring. Counseling should also be provided the on use of contraceptives, pregnancy planning, and postmenopausal hormone therapy. Dietary counseling for cardiovascular disease prevention and physical activity should also be encouraged.
Q: Is there a take-away for nurses who encounter this patient population?
“Nurses must remember and focus on how expansive this disease is-that it really can affect any vessel in the body. Pay attention to the signs and symptoms associated with antiphospholipid syndrome, and be prepared to implement cardiovascular disease management and education interventions. Also, continually counsel patients to stick with their medication.”




