Article
Oral Glucocorticoids and Fracture Risk in RA
Author(s):
Low-dose oral glucocorticoid therapy increases only vertebral fracture risk in rheumatoid arthritis patients, a study shows.
ASBMR Report: Vertebral Fractures increased With Low-Dose Glucocorticoids in RA
Low-dose oral glucocorticoid therapy increases only vertebral fracture risk in rheumatoid arthritis patients, according to a study presented on Sept. 15 at the American Society for Bone and Mineral Research (ASBMR) annual meeting which wrapped this week.
“Clinicians should be aware that even in rheumatoid arthritis patients who receive low daily glucocorticoid doses, clinical vertebral fracture risk is increased,” wrote study author Shahab Abtahi, M.D., MSc, of Maastricht University in The Netherlands, and colleagues.
Randomized clinical trials have shown that low-dose glucocorticoid therapy in patients with rheumatoid arthritis was associated with reduced bone mineral density loss in the hands or hip. But, the effect of low-dose glucocorticoid therapy on osteoporotic fractures is not clear, with observational studies reporting contrasting results compared to the bone mineral density trials.
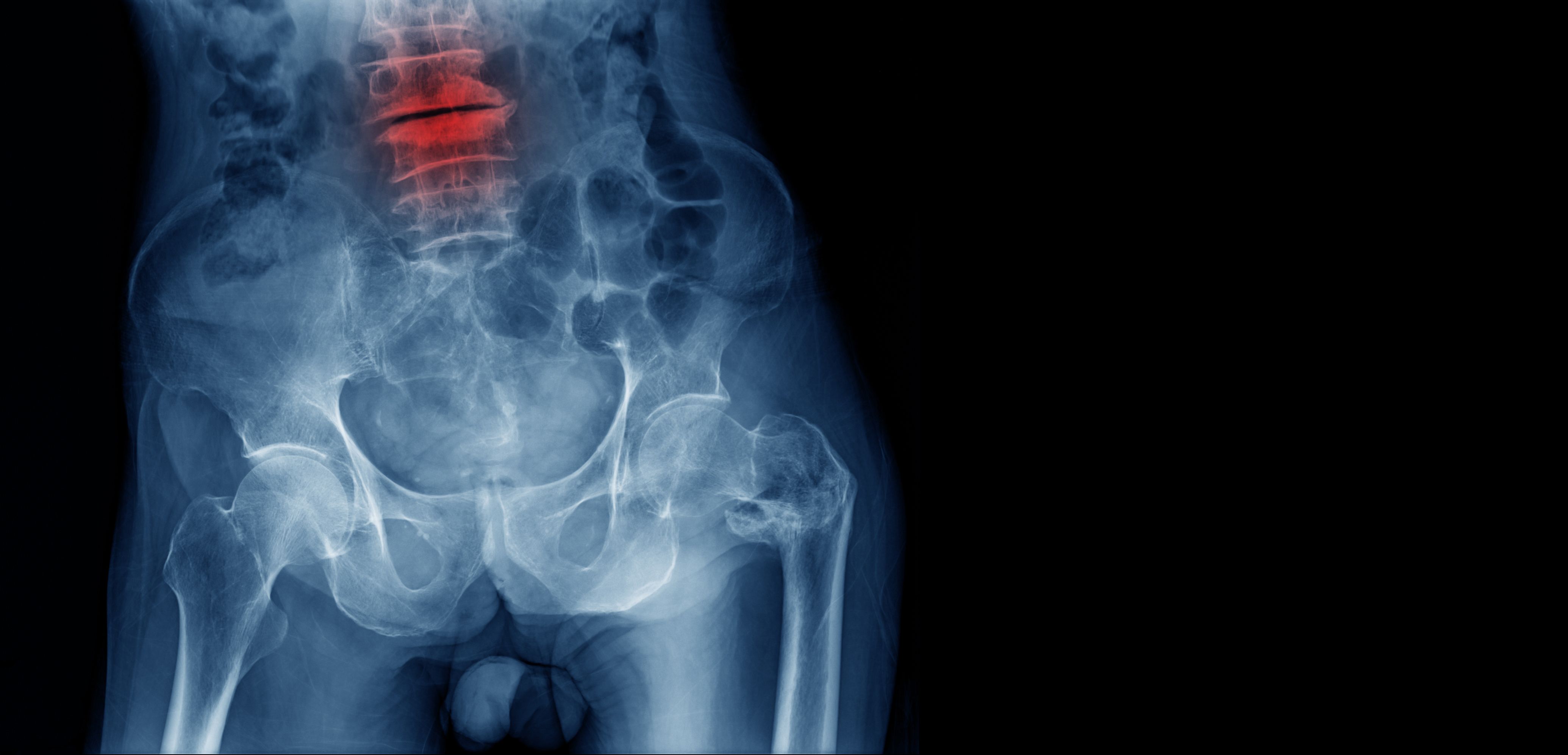
Dr. Abtahi and colleagues investigated the effects of low-dose (average daily dose ≤7.5mg prednisolone equivalent dose [PED]/day) oral glucocorticoid use on the risk of osteoporotic fractures at the hip, vertebrae, humerus, forearm, pelvis, and ribs in patients with rheumatoid arthritis aged over 50 years. They observed an increased risk with clinically vertebral fractures, but not with other fracture sites (non-vertebral).
This retrospective U.K. cohort study included 15,123 patients (mean age 68.8 years, 68 percent females) from 1997 to 2017. Oral glucocorticoid exposure was stratified based on the time since the most recent prescription, as current (<6 months), recent (7-12 months), and past use (>1 year). The analyses were adjusted for comorbidities, comedications and life-style parameters.
A total of 1,640 osteoporotic fractures occurred. Current low-dose oral glucocorticoid therapy was not associated with an increased risk of osteoporotic fracture compared with pastglucocorticoid use (adjusted hazard ratio 1.14, 95%CI 0.98-1.33). Among the six osteoporotic fractures studied, only clinical vertebral fracture had higher rates with low-dose glucocorticoid use (adjusted hazard ratio 1.59, 95%CI 1.11-2.29) versus past use. Meanwhile, high-dose (>7.5mg PED/d) long-term oral glucocorticoid therapy was associated with a 1.5-fold increased risk of osteoporotic fractures compared with past glucocorticoid therapy use.
“Our results are in line with findings from randomized clinical trials reporting a similar effect of low-dose glucocorticoid use on bone mineral density in various anatomical sites,” the authors wrote.
_______________
REFERENCE
[1115] The Effect of Low-dose Oral Glucocorticoid Therapy on Osteoporotic Fracture Risk in Patients with Rheumatoid Arthritis: the UK Clinical Practice Research Datalink. Shahab Abtahi. September 15. ASMBR 2020 Annual Meeting Virtual Event.




