Article
Pancreatic Cysts: Why Biopsies Fall Short
Author(s):
Pancreatic cancer is hard to cure and even diagnosing it is challenging. Among the eagerly awaiting research topics to be presented at the American College of Gastroenterology Meeting in Honolulu, Hawaii are reports on new developments in detecting malignancies.
Pancreatic cancer is hard to cure and even diagnosing it is challenging. Among the eagerly awaiting research topics to be presented at the American College of Gastroenterology Meeting in Honolulu, Hawaii are reports on new developments in detecting malignancies.
Due to embargo constraints, developers of a promising test that uses molecular analysis could not yet discuss their research, but they said their findings show such tests could significantly improve treatment of patients found to have these cysts.
Essentially, said Nancy Lurker, BS, MBA, chief executive of PDI, a Parsippany, NJ company that makes several molecular diagnositics, pancreatic cysts can be a precursor of pancreatic cancer--or they can indicate pancreatitis or other less serious conditions.
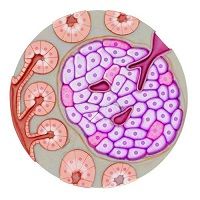
There are dozens of tubules that drain fluids from the pancreas, and when one stops draining, the backed-up fluid can show up on imaging as a cyst. “The plumbing system gets clogged,” Lurker said. Fortunately most of these cysts turn out to be benign, but pathologists can have a hard time diagnosing them. After an image of a cyst shows up, the next step in diagnosis is endoscopic ultrasound (EUS) in which a patient goes to an outpatient surgical facility and surgeons--using endoscopy and an image-guided needle--extract fluid from the cyst.
The procedure is invasive, with potential side effects and yet it can be inconclusive.
“In a few cases, it is clear the cyst is malignant,” she said, but often it is impossible to tell. Under past American Gastroenterology Association (AGA) guidelines, surgeons were to err on the side of caution and perform a Whipple procedure when they thought the cyst fluid might indicate cancer.
That meant that many patients went through this difficult surgery, one with many serious side effects, even though their pancreatic cysts turned out to be benign.
With the Whipple, “They cut off part of the stomach, the small intestine and sometimes the liver,” she said, “Patients become type 2 diabetics, they have GI problems, and there is a 2% to 5% mortality rate.”
For patients with malignant pancreatic tumors that may be a necessary price to pay, but not for patients who turn out not to have cancer. Accordingly, “The pendulum shifted and now the AGA recommends more watchful waiting,” she said.
Molecular testing at the time of endoscopic biopsy could save patients without malignancies from going through an unnecessary surgical ordeal. It also has the potential to detect malignancies earlier, giving pancreatic cancer patients a better shot at recovery or longer remissions.
The company will be presenting data Oct. 18 on their researchers' latest studies on their test’s accuracy.
That data will add new findings to a study published in February, 2015 that found that the company's test, PancraGen is 90% accurate in predicting benign and malignant disease in pancreatic cysts, she said.




