Article
The pathoanatomy of elbow fracture-dislocations: A road map to treatment
Elbow fracture-dislocations are complex injuries that encompass both soft tissue and bony injury. Recognizing the significance of the bony articulation, soft tissue complex, and support of the musculotendinous units is central to an understanding of the pathoanatomy. Four common patterns have been identified, 2 that are true dislocations with loss of ulnohumeral articulation and 2 that represent only an ulnohumeral disruption but warrant inclusion as elbow fracture-dislocations. Complications may be early (eg, instability and stiffness) or late (eg, arthrosis). Three anatomical components provide stability and facilitate elbow function: the osseous articulation, capsuloligamentous complex, and musculotendinous units. With each progressive stage of soft tissue injury, the elbow experiences increasing instability. Elbow fracture-dislocations require operative treatment. (J Musculoskel Med. 2008;25:53-62)
Elbow fracture-dislocations are complex injuries that encompass both soft tissue and bony injury. Recognizing the significance of the bony articulation, soft tissue complex, and support of the musculotendinous units is central to an understanding of the pathoanatomy. Four common patterns have been identified, 2 that are true dislocations with loss of ulnohumeral articulation and 2 that represent only an ulnohumeral disruption but warrant inclusion as elbow fracture-dislocations. Complications may be early (eg, instability and stiffness) or late (eg, arthrosis). Three anatomical components provide stability and facilitate elbow function: the osseous articulation, capsuloligamentous complex, and musculotendinous units. With each progressive stage of soft tissue injury, the elbow experiences increasing instability. Elbow fracture-dislocations require operative treatment. (J Musculoskel Med. 2008;25:53-62)
Elbow dislocations may be divided into 2 broad categories: simple dislocations and fracture-dislocations. The latter are complex injuries that encompass both soft tissue and bony injury to the elbow. The result is inherent instability in the intricate relationship and functioning of the distal humerus, proximal ulna, and radial head. Recognizing the significance of the bony articulation, soft tissue complex, and support of the musculotendinous units is central to an understanding of the pathoanatomy and can lead to improved outcomes.
Simple dislocations usually may be managed with closed reduction and early range of motion, with minimal sequelae.1 In contrast, fracture-dislocations often require operative treatment and are associated with several complications, such as instability and stiffness. Complications are best avoided by achieving sound soft tissue and bony repair, stable reduction of the articulations, and early motion.
In this article, we review the common patterns of elbow fracture-dislocations, elbow anatomy, the mechanism of injury, and the management and rehabilitation of these injuries. We also discuss management of the complications.
COMMON PATTERNS
There have been many descriptions of what defines an elbow fracture-dislocation. Ring and Jupiter2 reviewed their institutional experience and identified 4 common patterns: (1) posterior elbow dislocation with fracture of the radial head (Figure 1), (2) posterior elbow dislocation with fracture of the radial head and coronoid process (the “terrible triad”) (Figure 2), (3) anterior elbow dislocation with fracture of the olecranon (Figure 3), and (4) posterior elbow dislocation with fracture of the proximal ulna (posterior Monteggia fracture) (Figure 4).

Figure 1 –
A type 1 elbow fracture-dislocation with posterior dislocation and fracture of the radial head is seen in this x-ray film. Coronoid process integrity must be confirmed.

Figure 2 –
This type 2 elbow fracture dislocation represents the “terrible triad,” with a posterior elbow dislocation, coronoid fracture, and radial head fracture.

Figure 3 –
In a type 3 anterior or transolecranon fracture dislocation, the relationship of the radius and the ulnar shaft is maintained distally.

Figure 4 –
This type 4 injury represents a proximal posterior Monteggia fracture with posterior dislocation of the elbow.
Types 1 and 2 are true dislocations in which there is loss of ulnohumeral articulation. In types 3 and 4, the relationship between the ulna and humerus may be maintained; therefore, they represent an ulnohumeral disruption. Although type 3 and 4 injuries are not true dislocations, they result in sufficient disruption that their management and sequelae warrant their inclusion as elbow fracture-dislocations.
Complications after elbow fracture-dislocations may be divided into early and late. Early complications include instability, stiffness, and heterotopic ossification; late complications include fracture malunion/nonunion, radioulnar synostosis, and arthrosis. Understanding the fracture and institution of appropriate treatment, as well as having awareness of the complications, may help physicians optimize the results.
ANATOMY
Elbow anatomy illustrates an elegant balance between the functional requirements of positioning the hand in space and the stability required for manipulating objects, bearing weight, and throwing. Motion at the elbow may be broken down broadly into flexion-extension of the elbow and rotation of the hand at the wrist. Three anatomic components provide stability and facilitate elbow function: (1) the osseous articulation, (2) the capsuloligamentous complex, and (3) the musculotendinous units.
Osseous articulation
The elbow is a highly congruent joint that has significant inherent stability. The distal humerus is angled about 30° anteriorly and has 2 articulations: the capitellum and trochlea. The capitellum articulates with the radial head, providing rotation. The trochlea, which is covered by articular cartilage over an arc of 300° and is highly conformed to the proximal ulna, provides flexion-extension. This articulation alone is the predominant provider of elbow stability.3 The anterior angulation allows for increased flexion before impingement. An olecranon and coronoid fossa on the distal humerus allow for additional motion, as well as increased stability, with interlocking of their corresponding processes at the extremes of elbow motion.
Stability is further enhanced at the ulnohumeral articulation by the spool-shaped anatomy of the trochlea that interdigitates with the central groove in the corresponding ridge of the trochlear notch of the olecranon and the height of the coronoid process. Large coronoid fractures compromise the stability of the trochlear notch, as well as the integrity of the medial collateral ligament (MCL), which inserts at the base of the coronoid process at the sublime tubercle.4 Consequently, the ulnohumeral articulation provides significant stability in the anteroposterior plane of the elbow. In addition, the highly congruent nature of the ulnohumeral joint also provides varus-valgus and rotational stability.
The radial head also contributes to elbow stability while providing for rotation of the hand and force transmission. As much as 60% of a load seen by the hand is transmitted to the humerus through the radiocapitellar articulation.5 In addition, the radiocapitellar joint aids in resisting valgus stress. There is about a 30% decrease in the resistance to valgus load by the elbow with resection of the radial head.6 This valgus stability becomes paramount when the MCL is compromised.7 The radial head has been considered expendable when injured or dysfunctional, but in cases of concomitant injuries to the interosseous membrane of the forearm or MCL of the elbow, significant instability can ensue with its loss.
Capsuloligamentous complex
The MCL, which originates from the medial epicondyle and inserts on the ulna at the base of the coronoid process, has 3 components: the anterior, posterior, and transverse bundles. The posterior and transverse bundles are subtle thickenings of the medial joint capsule, but the anterior bundle is readily identifiable. Several studies that examined the valgus strength provided by the MCL suggested that the anterior band provides 33% to 50% of the resistance to valgus stress, depending on the amount of elbow flexion.6-9 MCL incompetence may occur in several forms, including frank rupture, chronic attenuation (as in throwing sports), and coronoid process or medial epicondyle fractures.
The lateral collateral ligament (LCL) originates from the lateral epicondyle and inserts on the annular ligament over the radial head and the ulna posteriorly. Its components include the radial collateral, annular, and accessory ligaments and lateral ulnar collateral ligament (LUCL). The LCL complex provides varus and posterolateral rotatory stability to the elbow; tension in the LCL complex and the overlying musculotendinous structures maintains apposition of the radial head to the capitellum.10,11 Incompetence of the LCL, and particularly of the LUCL component, has been used to explain recurrent elbow dislocation or instability through a posterolateral route without an associated fracture.
Musculotendinous units
The muscles crossing the elbow joint provide dynamic stability. Muscular contractures help maintain the ulnohumeral articulation. A cadaveric study showed that in elbows with sectioned MCL complexes, simulated physiological muscle action could partially restore normal joint kinematics.7
MECHANISM OF INJURY
In simple elbow dislocations, the articular relationship is disrupted by way of soft tissue injury. The injury begins laterally and extends medially, involving both the anterior and posterior soft tissue envelope. It has been described in 3 stages12: (1) the LCL complex is partially or completely torn (posterolateral subluxation), (2) anterior and posterior soft tissue is torn (posterolateral dislocation), and (3) the MCL complex is torn (true dislocation).
With each progressive stage of soft tissue injury, the elbow experiences increasing instability, from posterolateral subluxation to frank dislocation. As long as the anterior band of the MCL is left intact, the joint can be reduced and stability can be attained through reduction of the bony articulations, despite the significant soft tissue injury. In contrast, elbow fracture-dislocations incorporate both a ligamentous and a bony injury, eliminating the hopes of stability with reduction.
FRACTURE MANAGEMENT
In our opinion, elbow fracture-dislocations require operative treatment. Both the ligaments and fracture must be managed during treatment. Steps include reduction of the dislocation, management of the fracture (fixation vs replacement), and repair of the collateral ligaments.
Posterior dislocation with fracture of the radial head
Anteroposterior and lateral radiographs readily identify posterior elbow dislocation with associated radial head fracture. The x-ray film must be scrutinized initially for associated coronoid fracture, which may be evident as a small fragment in the soft tissue and may become incarcerated within the trochlear groove.
In the absence of a coronoid process fracture, treatment may be nonoperative or operative. Successful nonoperative treatment after closed reduction of elbow dislocations with fractures of the radial head has been reported.13 Nonoperative treatment includes gradual range of motion after a brief period of immobilization for minimally displaced radial head fractures without a block to forearm rotation.
With increasing severity of radial head injuries, operative fixation is recommended to avoid restricted forearm rotation and malunion. Displaced or comminuted fractures of the radial head traditionally have been excised. Recently improved understanding now indicates that a radial head fracture should be fixed or replaced when a ligamentous injury is suspected, as is the case with elbow dislocations, to avoid instability.6,7
For small displaced radial head fractures, we manage the fracture with internal fixation. In comminuted cases, radial head replacement is performed. A lateral approach is used to access the radial head. The LCL complex is evaluated and reattached to the lateral epicondyle with drill holes or suture anchors. The elbow also is evaluated medially; if the MCL is injured, it is examined and repaired. The ulnar nerve also may be released through this approach.
Posterior dislocation with fracture of the radial head and coronoid process
With the addition of a coronoid fracture, operative treatment becomes more involved. Ring and Jupiter2 advocated fixing all fractures of the coronoid process regardless of size because this injury has instability and historically poor treatment results.
Multiple exposures and fixation options are available for the coronoid process.14 We advocate a midline posterior approach, again facilitating access to both the medial and lateral sides. The coronoid fracture is approached first through the medial side.The ulnar nerve is identified and released. The split in the 2 heads of the flexor carpi ulnaris, through which the ulnar nerve travels, is used. The anterior head is raised off the ulna while the ulnar nerve is protected, exposing the coronoid process.
Fixation of the coronoid fracture can be accomplished with a suture passed through a drill hole or screw fixation from posterior to anterior. Attention is then turned laterally, where the radial head is repaired or replaced and the LCL is repaired (Figure 5). Stability is checked through examination of range of motion. If there is instability in the midrange of motion, a hinged external fixator may be applied.
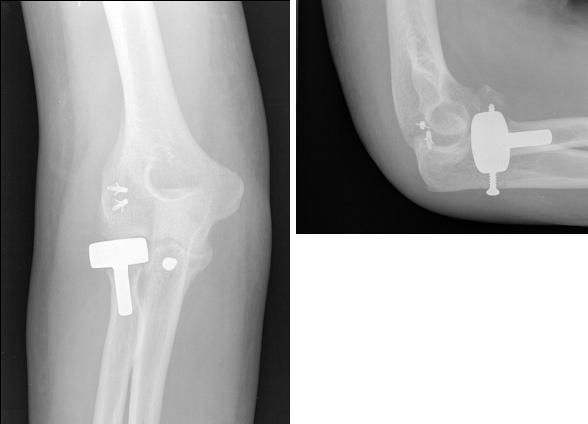
Figure 5 – Shown here is a type 2 “terrible triad” injury after the patient underwent open reduction, internal fixation of the coronoid fracture; radial head replacement; and repair of the lateral collateral ligament complex with suture anchors, resulting in a stable and congruent joint.
Anterior dislocation with fracture of the olecranon
The elbow dislocates anteriorly with anterior olecranon fracture-dislocations occurring through the proximal ulna, most often transolecranon. This pattern is easily confused with an anterior Monteggia fracture (fracture of the proximal ulnar shaft with radial head dislocation) but is distinguished by the radius and ulna both dislocating anteriorly and maintaining their relationship.15 Although this injury is not a true dislocation of the ulnohumeral joint, ulnohumeral articulation stability is disrupted and it should be managed as a fracture-dislocation of the elbow.
Fracture of the proximal ulna often is complex and may be associated with a large coronoid fragment. In contrast, the capsuloligamentous restraints may remain intact because the dislocation occurs predominantly from loss of osseous articulation rather than ligamentous incompetence.
We use a midline posterior approach. The coronoid is visualized directly through the olecranon fracture and fixed with screws. The olecranon is then reduced. The surgeon performs fixation of the ulna with plates and screws applied to the dorsal surface of the ulna while wrapping around the olecranon proximally. Often significant comminution is seen in the proximal ulna; it should be bridged with a plate of adequate length. Although the injury is severe, 15 of 17 patients in a Ring and associates15 series treated as outlined above achieved good or excellent results.
Posterior dislocation with fracture of the proximal ulna
Posterior olecranon fracture-dislocations may be considered part of the spectrum of posterior Monteggia fractures.15,16 The pattern includes a proximal ulna fracture, again often transolecranon, with apex posterior angulation of the fracture and posterior dislocation of the radial head. Again, although the injury is not a true dislocation, the stability of the ulnohumeral articulation is disrupted sufficiently to warrant its inclusion.
In addition to the proximal ulna fracture and a possible coronoid fracture, the radial head dislocates posteriorly and often is fractured. The LCL also is often injured, predisposing to posterolateral rotatory instability.
We use a midline posterior approach. The coronoid is examined through the proximal ulna fracture and fixed with screws. The radial head is repaired or replaced and then reduced. The LCL is repaired. The ulna is plated.
In a Jupiter and colleagues16 study of 11 cases of posterior Monteggia lesions, 6 had good or excellent results. The inferior results were related to inadequate reduction of the ulna and coronoid, with persistent posterior subluxation of the radiocapitellar joint.
REHABILITATION
The intraoperative goal is restoration of elbow stability. If this is achieved, then early motion can be instituted after a brief (less than 2 weeks) period of immobilization. When fixation is more tenuous or stability is guarded, the period of immobilization may have to be increased or, preferably, motion may be initiated with the protection of a hinged elbow fixator applied externally.
COMPLICATIONS
Instability
Early instability after operative fixation is best managed with diligent examination under fluoroscopy intraoperatively. In addition, adequate reduction and fixation of the fracture and ligamentous repair must be reconfirmed. In the presence of persistent instability, a hinged external elbow fixator may be applied. In contrast, chronic instability may be the result of malunion, nonunion, bony defects, or attenuation or inadequate repair of the soft tissue.
Stiffness
Loss of motion is common after any elbow injury, including both simple and complex dislocations. Immobilization for longer than 2 weeks has been shown to greatly increase the risk of stiffness, which is best avoided with early motion.1 Prolonged immobilization would be considered after elbow fracture-dislocations only if the repair was tenuous. In this situation, both protection of the repair and early immobilization are best managed with a hinged elbow fixator.
Stiffness after fracture healing may be managed with static progressive splinting. Open release of the elbow capsule also may be used; assuming that the articular anatomy is well-reduced, the chances of success are good.17
Heterotopic ossification
Risk factors for heterotopic ossification include severe trauma, burns, and brain injuries.18 Other, less well defined risk factors include the patient’s sex and genetic makeup.
The relationship between operative management of elbow fracture-dislocations and the risk of heterotopic ossification remains controversial. Traditionally, early operative fixation was thought to increase the risk. More recently, the timing of surgery and the risk of heterotopic ossification have been shown to be unrelated.19
In the trauma and joint arthroplasty literature, radiation therapy and NSAIDs have been shown to be effective against heterotopic ossification.20 Use of these modalities must be tempered with consideration of the risk of compromised wound healing with radiation therapy and of medical morbidity with NSAIDs.
Resection of heterotopic ossification is successful in returning motion, but the timing of surgery historically has been controversial. Early resection avoids formation of elbow contractures and joint degeneration but risks return and exacerbation of the process. In cases of isolated elbow trauma without head injury, resection has been shown to be successful without recurrence when the heterotopic bone assumes a well-defined trabecular pattern on plain radiographs.21,22
Arthrosis
Posttraumatic arthrosis occurs as a result of severe injury, articular injury, and residual instability. Treatment of patients with symptomatic arthrosis resistant to nonoperative management is directed by their age. Total elbow arthroplasty is effective in treating older patients, in whom there are fewer demands on the involved extremity.23 In younger patients, debridement and fascial interposition arthroplasty may allow for maintenance of a more active lifestyle.24
References:
References
- 1. Mehlhoff TL, Noble PC, Bennett JB, Tullos HS. Simple dislocation of the elbow in the adult: results after closed treatment. J Bone Joint Surg. 1988;70A:244-249.
- 2. Ring D, Jupiter JB. Fracture-dislocation of the elbow. J Bone Joint Surg. 1998;80A:566-580.
- 3. Morrey BF. Anatomy of the elbow joint. In: Morrey BF, ed. The Elbow and Its Disorders. 3rd ed. Philadelphia: WB Saunders; 2000:13-42.
- 4. Cage DJ, Abrams RA, Callahan JJ, Botte MJ. Soft tissue attachments of the ulnar coronoid process: an anatomic study with radiographic correlation. Clin Orthop Rel Res. 1995;320:154-158.
- 5. Halls AA, Travill A. Transmission of pressures across the elbow joint. Anat Rec. 1964;150:243-247.
- 6. Hotchkiss RN, Weiland AJ. Valgus stability of the elbow. J Ortho Res. 1987;5:372-377.
- 7. Morrey BF, Tanaka S, An KN. Valgus stability of the elbow: a definition of primary and secondary constraints. Clin Orthop Rel Res. 1991;265:187-195.
- 8. Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11:315-319.
- 9. Sojbjerg JO, Ovesen J, Gundorf CE. Experimental elbow instability after transection of the medial collateral ligament. Clin Orthop Rel Res. 1987;218:186-190.
- 10. O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow. J Bone Joint Surg. 1991;73A:440-446.
- 11. Cohen MS, Hastings H 2nd. Rotatory instability of the elbow: the anatomy and role of the lateral stabilizers. J Bone Joint Surg. 1997;79A:225-233.
- 12. O’Driscoll SW, Jupiter JB, Cohen MS, et al. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113-134.
- 13. Broberg MA, Morrey BF. Results of treatment of fracture-dislocations of the elbow. Clin Orthop Rel Res. 1987;216:109-119.
- 14. Ring D. Fractures of the coronoid process of the ulna. J Hand Surg. 2006;31A:1679-1689.
- 15. Ring D, Jupiter JB, Sanders RW, et al. Transolecranon fracture-dislocation of the elbow. J Orthop Trauma. 1997;11:545-550.
- 16. Jupiter JB, Leibovic SJ, Ribbans W, Wilk RM. The posterior Monteggia lesion. J Orthop Trauma. 1991;5:395-402.
- 17. Husband JB, Hastings H 2nd. The lateral approach for operative release of post-traumatic contracture of the elbow. J Bone Joint Surg. 1990;72A:1353-1358.
- 18. Garland DE. A clinical perspective on common forms of acquired heterotopic ossification. Clin Orthop Rel Res. 1991;263:13-29.
- 19. Noblin JD, Geissler WB, Bass D. The incidence of heterotopic ossification with elbow injuries. Orthop Trans. 1995;19:162.
- 20. Kjaersgaard-Andersen P, Ritter MA. Prevention of formation of heterotopic bone after total hip arthroplasty. J Bone Joint Surg. 1991;73A:942-947.
- 21. Jupiter JB, Ring D. Operative treatment of post-traumatic proximal radioulnar synostosis. J Bone Joint Surg. 1998;80A:248-257.
- 22. McAuliffe JA, Wolfson AH. Early excision of heterotopic ossification about the elbow followed by radiation therapy. J Bone Joint Surg. 1997;79A:749-755.
- 23. Morrey BF, Adams RA, Bryan RS. Total replacement for post-traumatic arthritis of the elbow. J Bone Joint Surg. 1991;73B:607-612.
- 24. Morrey BF. Post-traumatic contracture of the elbow: operative treatment, including distraction arthroplasty. J Bone Joint Surg. 1990;72A:601-618.




