Article
Patients with RA Hesitant to Make Changes to DMARD Therapy
Author(s):
Investigators believe that treatment escalation within patients with rheumatoid arthritis should utilize interventions beyond the traditional physician-patient relationship.
While patients have varying opinions about their rheumatoid arthritis (RA) treatment, apprehension regarding adding or switching disease-modifying antirheumatic drugs (DMARDs) was present among all patients, even for those who understood the benefits associated with DMARDs and had access to high quality care and support. According to the study “Understanding heterogeneity in patients’ conceptualization of treatment for rheumatoid arthritis: A cluster analysis,” which was presented at the European Alliance of Associations for Rheumatology (EULAR) 2022 conference, investigators believe that treatment escalation within this patient population should utilize interventions beyond the traditional physician-patient relationship.
“Uptake of treat to target strategies for the management of RA is low,” investigators stated. “System- related barriers to accessing treatment are known, but poor adherence to starting and continuing treatment are prevalent causes of suboptimal care.”
Patients registered in the ArthritisPower US online research registry were eligible to participate in the study if they had both clinically diagnosed RA and were currently being treated with 1 or more DMARDs. Participants rated 56 items, on a scale of 1 to 5, to determine the heterogeneity of patient’s conception of RA treatment to inform interventions that may ultimately improve DMARD adherence. Questions reflected concepts raised during patient interviews. A principal components analysis using Varimax rotation was used to combine similar items in order to analyze and interpret the results more easily. Mean scores were entered into a k-means cluster analysis and any patterns within demographic characteristics across clusters were evaluated.
The 621 patients included in the study had a mean age of 57 years (ranging from 22 to 93 years), 89% were female, and 89% were non-Hispanic White. Approximately a quarter (27%) of patients self-reported obtaining a post-graduate degree. According to a scree plot, there was a 4-factor solution that explained 36.8% of the variance for optimal interpretability.
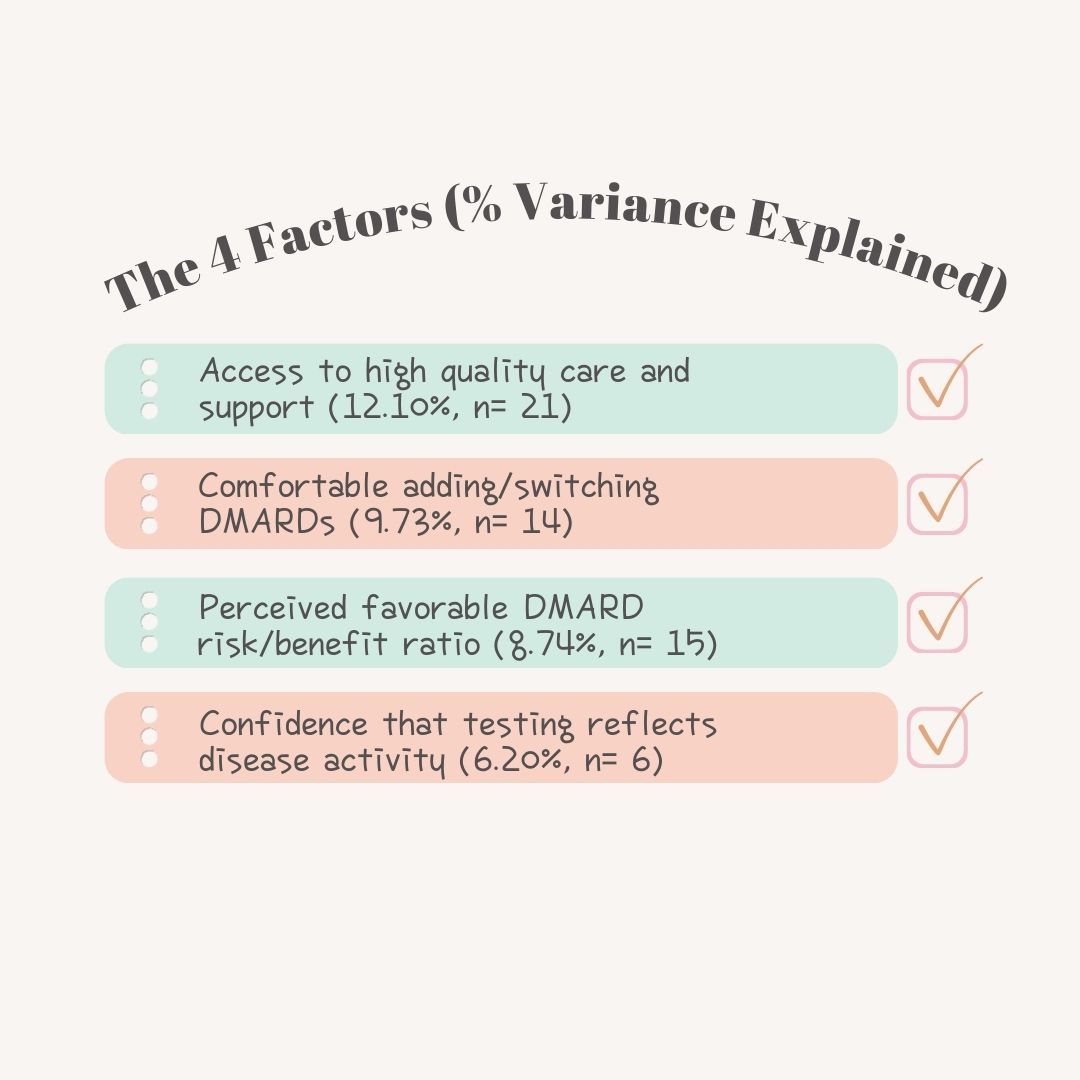
The 5-cluster solution revealed the most stable convergence of cluster centers, with the largest group (31.7%) characterized by mean scores on each of the 4 factors reflecting positive experiences, labeled “Successfully Engaged in Care.” This reflects a positive relationship with a rheumatologist and patients that felt both informed and had an active role in care. The second group, labeled “Worried About Medication,” had high scores in both Factor 1 (access to high quality care and support) as well as Factor 3 (those who felt favorably about the DMARD risk/benefit ratio), but were still not comfortable in adding or switching DMARDs and had less certainty in the role of testing to reflect their disease activity. Cluster 3 (16.4%), labeled “Skeptical of Testing,” had a positive view of DMARDs but presented lower scores related to Factor 1 and Factor 4 (confidence in testing). Cluster 4, labeled “Resistant to DMARDs,” (14.3%) exhibited a low perceived value of DMARDs and had lower scores for DMARD risk/benefit as well as confidence in testing. The final cluster, labeled “Dissatisfied with Care,” (13.2%) had the lowest rating of access to quality care and did not feel supported in their decision making. However, the patient-reported risk/benefit ratio of DMARDs treatment was still favorable.




