Article
Polypharmacy Gains Favor in Lupus Nephritis
Simultaneous use of more than one drug is gaining traction as a treatment strategy for severe lupus symptoms, particularly in people with chronic kidney disease.
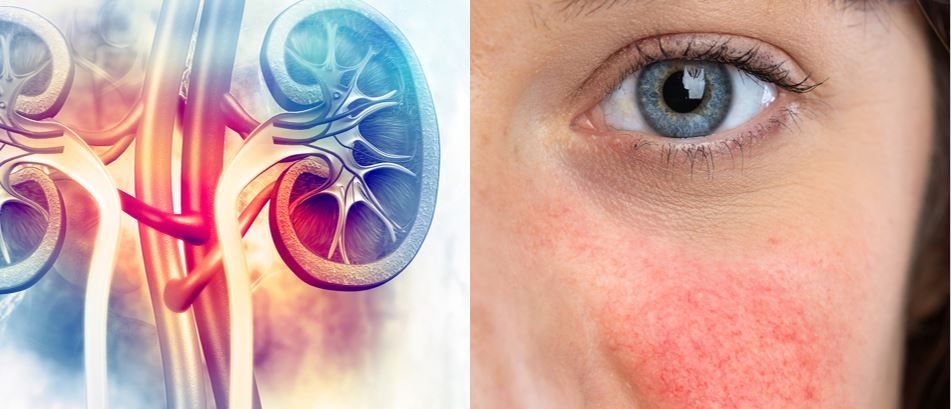
Simultaneous use of more than one drug is gaining traction as a treatment strategy for severe lupus symptoms, particularly in lupus patients with chronic kidney disease.
That’s according to a physician-scientist who recently presented at the Congress of Clinical Rheumatology East 2020 annual meeting.
"Right now, we don’t know a way to treat at-risk patients differently with different drugs,” said Joan Merrill, M.D., a physician-researcher with the Clinical Pharmacology Research Program at the Oklahoma Medical Research Foundation of the University of Oklahoma. “We don’t have that level of sophistication to know how to select whether patients should they get cyclophosphamide or azathioprine. In lupus nephritis we're beginning to see the use of polypharmacy with more frequency. Patients with a worse prognosis are probably going to want to go more quickly to polypharmacy to try and get kidney disease under control faster.”
Dr. Merrill identified several phenotypes associated with higher risks, including gender (women are far more likely to develop the disease) and race. In the latter, the prevalence of lupus per 100,000 population is: Northern European: 5.6 (CI 4.6-6.7), Indian Asian: 21.4 (CI 12-35.2), African-Caribbean: 99.2 (CI 55.5-163.6), and Chinese: 110.3 (CI 55-197.3), according to study data. She also called chronic kidney disease “a phenotype to avoid,” and one that may justify trying polypharmacy.
“Even when you’re only at stage two [of chronic kidney disease], after 10 years, 20 percent of those patients have died,” she said. “Let’s remember that chronic kidney disease is the absolute worst phenotype that we would like to prevent. And I would tend to think that as long as we’re doing things empirically, we’re going to watch the literature and see which drugs help the most patients when used together, as opposed to alone or in other combinations. And that’s going to be evolving.”
______________
REFERENCE
9/11, 9 a.m: “Phenotypes in SLE: Can They Predict Characteristic, Disease Outcomes and Treatment Needs?




