Article
Post-PCI Bivalirudin Extended Duration Shows No Benefits
Author(s):
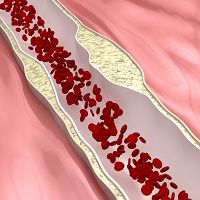
Researchers who assessed patients undergoing percutaneous coronary intervention (PCI) reported that extending the use of a particular anti-clotting medication following the procedure did not lead to additional benefits.
Researchers who assessed patients undergoing percutaneous coronary intervention (PCI) reported that extending the use of a particular anti-clotting medication following the procedure did not lead to additional benefits.
Lead investigator Marco Valgimigli, MD, PhD, and colleagues studied bivalirudin in patients with acute coronary syndrome. The results were presented at the European Society of Cardiology (ESC) Congress conference in London, UK, as well as published in The New England Journal of Medicine.
A total of 3,610 patients with acute coronary syndrome were randomly assigned either bivalirudin only during PCI (1,188 patients) or both during and after PCI (1,799 patients). Bivalirudin was administered with a bolus of 0.75 mg per kilogram and immediately followed by 1.75 mg per kilogram each hour until the end of PCI, as recommended on the label. Those who received the prolonged treatment could either receive, as decided by the physicians, the full dose for four hours after PCI or the lower dose of 0.25 mg per kilogram per hour for at least six hours.
“Both treatment options are allowed per current European label and observational studies,” Valgimigli, of the Swiss Cardiovascular Center, said in a news release.
For 30 days following the procedures, the team assessed primary outcomes, including urgent target vessel revascularization, definite stent thrombosis, and net adverse clinical events. The rates proved to be similar between the groups, occurring in 11% of those who received post-PCI bivalirudin and 11.9% of those who did not receive the medication following the procedure. Bleeding was measured using the BARC (Bleeding Academic Research Consortium), TIMI (Thrombolysis In Myocardial Infarction), and GUSTO (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries).
“Hence, I believe the option to prolong or stop bivalirudin infusion after PCI remains open for clinicians,” Valgimigli continued, “who will have to decide based on the ischemic and bleeding risk of individual patients as well as perhaps based on type of acute coronary syndrome, timing of loading dose and type of oral P2Y12 inhibitors.”
In addition, both the 1.75 mg and 0.25 mg post-PCI bivalirudin doses seemed to be treatment modifiers.
“I would like to caution against the over interpretation of these results as the choice of post-PCI bivalirudin regimen was not randomized, but rather left to the discretion of the investigators,” Valgimigli concluded. “However, taking these words of caution into great account, what we saw is that the full dose regimen may be able to significantly reduce stent thrombosis risk without increasing bleeding. This may be in keeping with previous observations from the EUROMAX trial.”





