Article
PRAGUE-12 at 5 Years: Stroke Rate Reduced, Sinus Rhythm Maintained
Author(s):
The 5-year PRAGUE-12 study outcomes show that LAA ablation in cardiac surgery patients with a history of atrial fibrillation reduces stroke rate vs cardiac surgery alone.
The addition of surgical ablation to cardiac surgery in patients with atrial fibrillation (AF) increased the chance of maintaining sinus rhythm and reduced risk of stroke at 5 years, according to PRAGUE-12 study lead author Pavel Osmancik, MD, PhD, of the Charles University and University Hospital Kralovske Vinohrady, in Prague, Czech Republic. Dr Osmancik presented the long-term outcomes of the PRAGUE-12 study at the recent 2019 Heart Rhythm Society Meeting in San Francisco.
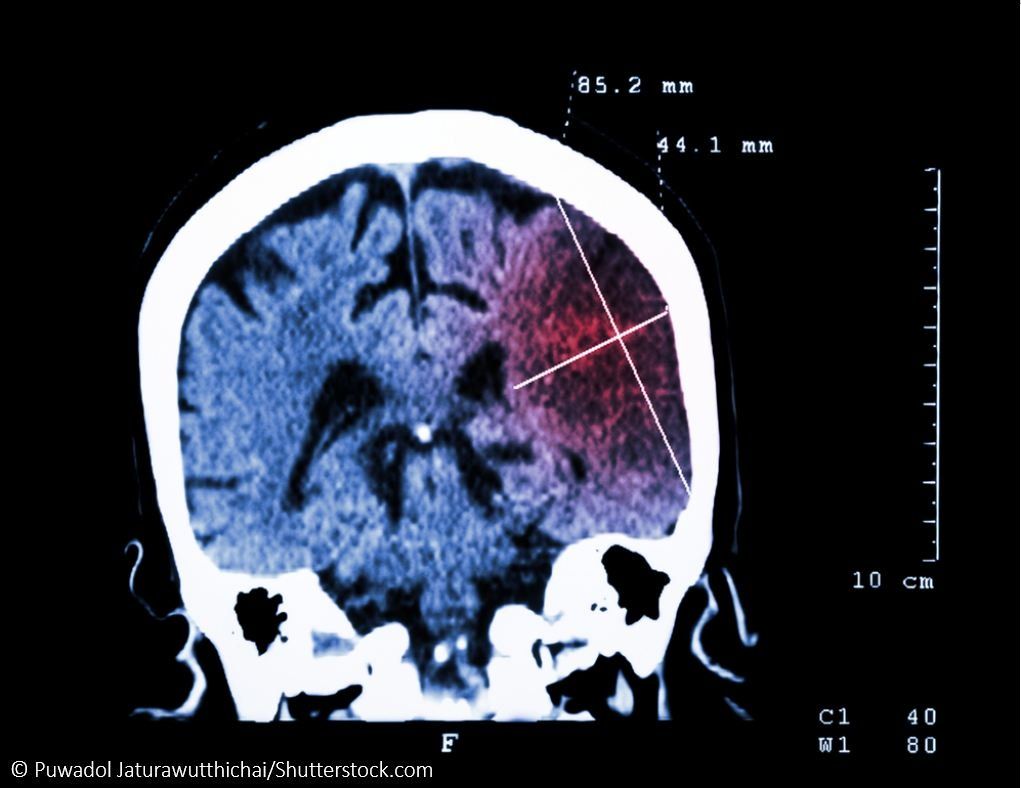
Atrial fibrillation, an independent risk factor for all-cause mortality, stroke, heart failure. and increased hospitalizations, is found in about 10% of all patients with indications for cardiac surgery and 2% of the general population.
The PRAGUE-12 study was a prospective, randomized clinical trial to assess a protocol of coronary artery disease (CAD) surgery or valve surgery plus ablation for AF vs cardiac surgery alone, over a 5-year follow up period. The one-year results first presented in 2012 showed that ablation was safe, Dr. Osmancik said, adding that “secondly, the ablation was effective in terms of having more sinus rhythm at one year...but there was no clinical effect.” The study's primary endpoint was a composite of cardiovascular (CV) death, stroke, hospitalization for heart failure or severe bleeding. Secondary endpoints included the elements of the primary endpoint plus AF recurrence.
At the end of 5 years, a total 108 patients had been treated with surgical ablation plus appendage exclusion using the MAZE procedure, compared to 99 who underwent surgery alone. Among surgical patients who also had ablation, the composite endpoint was observed less frequently than in those having surgery alone, although the difference was not significant after adjusting for competing risks.
While all components of the composite primary endpoint (CV death, stroke, hospitalization for heart failure, severe bleeding) were less frequent in number in the ablation group, only the difference in stroke reached statistical significance (5.6% vs 14.1%; SHR 0.32; 95% CI 0.12-0.84).
An important finding in the secondary endpoint analysis, Dr. Osmancik said, was that “the incidence of stroke was decreased in surgically ablated patients, and this decrease remained significant even after adjustment for all covariables including history of myocardial infarction and coronary artery disease.”
Dr Osmancik proposed that all patients who are candidates for cardiac surgery with a history of AF should also undergo surgical ablation since older trials have confirmed the procedure’s safety and efficacy in achieving sinus rhythm “But now,” he added, “we can also see that in the long term it [ablation] is associated with better survival, at least with decreased rate of stroke in the future.”
Source: Osmancik P, Budera P, Talavera D, et al. Five-year outcomes in cardiac surgery patients with arrial fibrillation undergoing concomitant surgical ablation versus no ablation: The long-term follow-up of the PRAGUE-12 study. Heart Rhythm (2019), doi: https://doi.org/10.1016/j.hrthm.2019.05.001.





