Article
Predisposition to Bone Mineral Density Determines Fracture Risk
Author(s):
A patient's genetic predisposition to low bone mineral density can increase their risk for osteoporotic fractures, according to a new genome-wide association study.
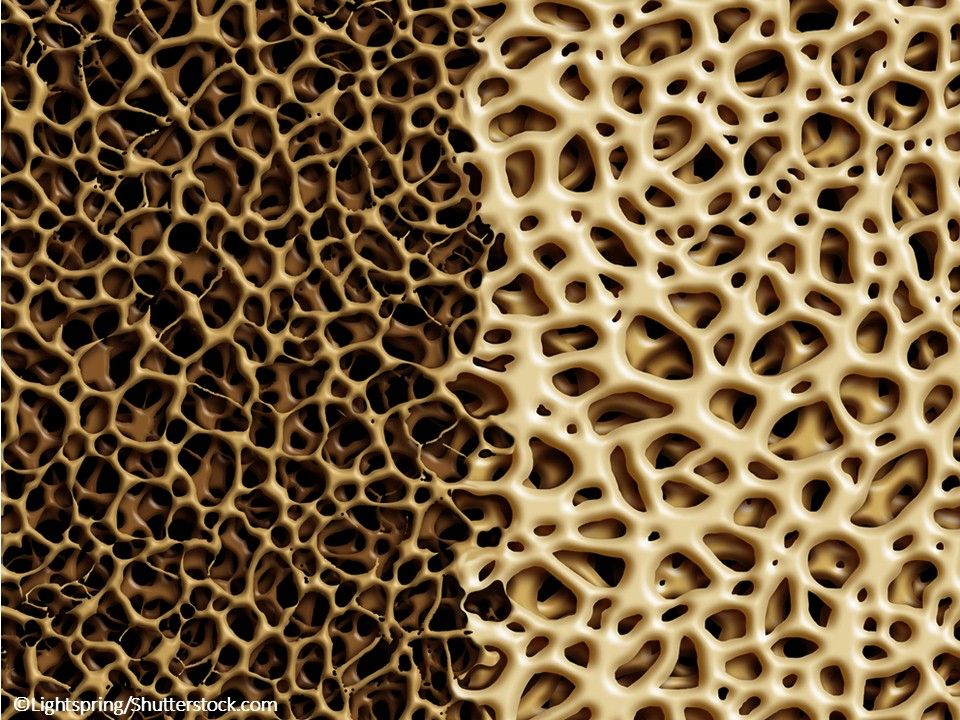
©Lightspring/Shutterstock.com
A genetic predisposition to low bone mineral density (BMD) plays a potential causal role in osteoporotic fracture risk, but lower levels of vitamin D and estimated calcium intake from dairy sources do not, according to a new study in the British Medical Journal.
This first genome-wide association study of fracture risk provides insight into the biologic mechanisms leading to fractures. All of the identified genomic regions found to be associated with fracture have also been previously found to be associated with variation in BMD.
The findings strongly suggest that treatments aimed at increasing bone strength are more likely to be successful in preventing fractures vs widespread supplementation of calcium and vitamin D or targeting other risk factors that were not found to mediate the disease.
“Among the clinical risk factors for fracture assessed in the study, only BMD showed a major causal effect on fracture. The genetic factors contributing to fractures are also the same ones that affect BMD,” said co-senior author Douglas P. Kiel, MD, MPH, of Harvard Medical School, Boston, Massachusetts. “Knowing one's genetic risk for fracture at an early age could be a useful piece of information to persons wanting to maintain their bone health as they age. Also, the study identified novel genetic variants that could be used to target future drug therapies to prevent fracture.”
The large international collaboration used data from 37 857 fracture cases and 227 116 controls and identified 15 variations in the genome that are related to the risk of bone fractures. The findings were replicated in 147 200 fracture cases and 150 085 controls.
All 15 of the fracture-associated loci identified were associated with BMD and mapped to genes clustering in pathways known to be critical to bone biology or novel pathways. Mendelian-randomization analyses showed a clear effect of BMD on fracture risk. One standard deviation decrease in genetically determined BMD of the femoral neck was associated with a 55% increase in fracture risk.
Hand grip strength, which is a surrogate for muscle mass, was inversely associated with fracture risk, but this result was not significant after multiple testing corrections. The remaining clinical risk factors, including vitamin D levels, showed no evidence for an effect on fracture.
“Despite high statistical power, none of the other tested and well accepted risk factors (eg, rheumatoid arthritis and other causes of secondary osteoporosis) or any of the other clinically relevant risk factors (vitamin D levels, dairy food derived calcium intake, fasting glucose, type 2 diabetes, and coronary heart disease) had evidence of a major causal effect on fracture risk,” the researchers wrote.
Vitamin D supplementation is part of clinical guidelines, but recent randomized controlled trials have failed to consistently demonstrate a beneficial effect. The researchers encourage clinicians to focus on building bone density as a more effective preventive measure against fracture.
They concluded that, “these results highlight the central causal role of low BMD in the pathophysiology of fracture risk.”





