Article
Primary Hyperparathyroidism Pearls
Primary hyperparathyroidism--asymptomatic but curable. Here are three clinical pearls to help guide diagnosis and management.
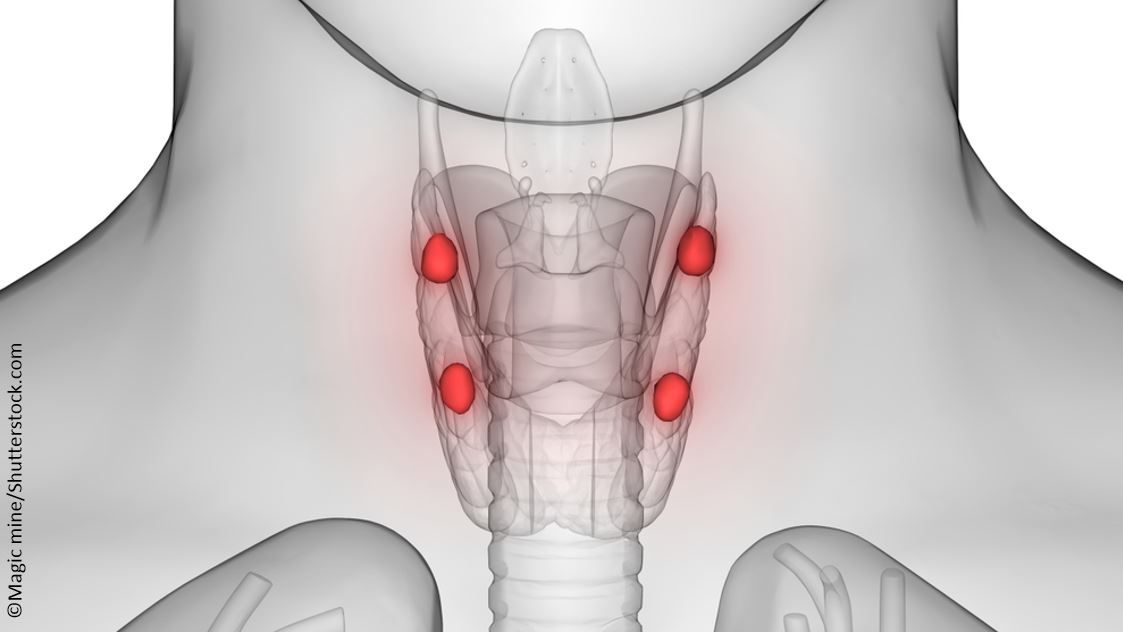
©Magic mine/Shutterstock.com
What is an endocrinologic condition in which patients are usually asymptomatic, yet can be cured?
Primary hyperparathyroidism (PHPT), a condition that is diagnosed in about 100,000 Americans per year, holds this distinction.
You remember the old mnemonic: “Bones, stones, abdominal groans, and psychic moans.” Routine and widespread checking of chemistry panels has largely rendered the above constellation of symptoms a historic relic, as the vast majority of patients with PHPT are asymptomatic at diagnosis. Yet, if present, the clinical manifestations can be protean.
Here are some clinical pearls to keep in mind if you see a patient with an elevated serum calcium.
1. Ask yourself, “Is that parathyroid hormone (PTH) inappropriately elevated (or inappropriately normal)?”
Your patient has a serum calcium of 11.8 mg/dL, so you order an intact parathyroid hormone (iPTH) level. If the PTH is 75 pg/mL, be sure to pause for a moment, and reflect on the lab values. If the patient is hypercalcemic, would the PTH be suppressed? Should it be? Thus, you would expect high, or even normal PTHs, and you know that this picture is consistent with PHPT.
As with virtually everything in medicine, and life in general, the story does not end there. A curveball that can complicate diagnosing PHPT is normocalcemic hyperparathyroidism (HPT). Using a nomogram, a study of 1753 patients with PHPT and 74 healthy controls found in the PHPT group, 70% had a typical clinical picture consistent with PHPT - namely, a concomitant elevation of both calcium (≥10.5 mg/dL) and PTH (≥65 pg/dL);1 21% fit the normocalcemic HPT, with calcium ≤10.5 mg/dL and PTH ≥65 pg/dL. A third group was the inversion of this, normal PTH, but with high calcium: 6% demonstrated a serum calcium ≥10.5 mg/dL and PTH ≤65 pg/dL. The last group (3%) was normal for both calcium and PTH.
2. Be vigilant for those familial hypocalciuric hypercalcemia (FHH) patients!
Granted, FHH is a very rare condition - it’s thought to afflict only about 1 in 78,000 individuals (compared with 1 in 1,000 for PHPT). An autosomal dominant disease, it is due to mutations in the calcium-sensing receptor gene. Please be sure to order a 24-hour urine calcium. Why? Surgery for an individual with FHH is not indicated, as the hypercalcemia would persist. A challenge can arise if there’s an atypical presentation of either FHH or PHPT.
3. What’s the best localization study?
You may have heard the old saying, “The best localization study for a PHPT patient is finding a great surgeon!” A sestamibi scan and ultrasonography are not recommended for diagnosing this condition. The surgeon may later obtain these to assist him or her.
For more details, please see the American Association of Clinical Endocrinologists’ Position Statement, as well as the NIH Consensus Development Conference on the Management of Asymptomatic Primary Hyperparathyroidism.
References:
- Lavryk OA, Siperstein AE. Use of calcium and parathyroid hormone nomogram to distinguish between atypical primary hyperparathyroidism and normal patients. World J Surg. 2017;41:122-128.
- AACE/AAES Task Force on Primary Hyperparathyroidism. The American Association of Clinical Endocrinologists and the American Association of Endocrine Surgeons Position Statement on the Diagnosis and Management of Primary Hyperparathyroidism. Endocr Pract. 2005;11:49–54.
- Khan AA, Bilezikian JP, Potts JT. The diagnosis and management of asymptomatic primary hyperparathyroidism revisited. J Clin Endocrinol Metab. 2009;94:333–334.
- Bilezikian JP, Khan AA, Potts JT. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Third International Workshop. J Clin Endocrinol Metab. 2009;94:335–339.




