Article
Promising New Molecule in HIV Vaccine Design
Author(s):
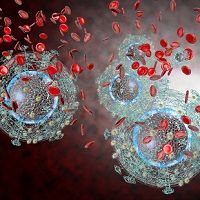
It's significant to produce antibodies directly targeting the defensive sugar shield in order to develop immunity against the target.
A new protein-sugar vaccine candidate demonstrated encouraging results, according to recent study from researchers at Duke University and the University of Maryland (UMD).
According to study the outcomes, Lai-Xi Wang of UMD and colleagues designed the vaccine candidate to initiate an immune response against the “sugar shields” that protect HIV and allow it to maintain its defenses.
Previous research into this type of vaccine has been hindered by similarities of the HIV sugar shield to standard sugars already found in the human body. The proliferation of HIV strains (more than 60), as well as their countless and constant mutations, can also make it difficult for a vaccine candidate to show efficacy across multiple strains.
“An obstacle to creating an effective HIV vaccine is the difficulty of getting the immune system to generate antibodies against the sugar shield of multiple HIV strains,” said Wang, a professor of chemistry and biochemistry, UMD. “Our method addresses this problem by designing a vaccine component that mimics a protein-sugar part of this shield.”
Wang and colleagues focused on combining a sugar molecule with a fragment of protein from gp120, which covers HIV and protects it. Both of these vaccine candidate elements are common among many strains of HIV. The research team used a synthetic chemistry method they previously developed to combine the gp120 fragment with the sugar molecule, and mimic the sugar shield.
Rarely do HIV-infected patients who don’t take medication naturally, produce the antibodies to attack gp120 and keep the virus at bay. However, in rabbit models, the vaccine candidate helped the immune system generate antibodies that bound to gp120 and protected against the sugar shields in 4 separate current, common, and active HIV strains.
Use of the protein fragment alone without the addition of the sugar molecule bound to gp120 from only 1 strain of HIV.
“This result was significant because producing antibodies that directly target the defensive sugar shield is an important step in developing immunity against the target and therefore the first step in developing a truly effective vaccine,” Wang said.
Though the vaccine stimulated protective antibodies in rabbits, live HIV was still able to infect cells. Wang says this is to be expected, as his animal study went on for only 2 months and it can take humans up to 2 years to build immunity against HIV.
“We have not hit a home run yet,” Wang noted. “But the ability of the vaccine candidate to raise substantial antibodies against the sugar shield in only 2 months is encouraging; other studies took up to 4 years to achieve similar results. This means that our molecule is a relatively strong inducer of the immune response.”
In the future, the research team plans to conduct longer-term studies, including tests of other vaccine candidate combinations in an effort to determine which specific areas of gp120 the antibodies are able to bind to, as well as learn how they can increase the antibodies’ ability to fight HIV.
The study, “Synthetic Three-Component HIV-1 V3 Glycopeptide Immunogens Induce Glycan-Dependent Antibody Responses,” was published in Cell Chemical Biology on Oct. 26, 2017.
Related Coverage
Study: Neutralizing Antibodies May Harm Babies of HIV-Positive Mothers
HIV Discovered Hiding in Overlooked Memory T Cells
Once Daily Single-Tablet HIV-1 Therapy Achieves Primary Endpoint





