Article
A Rare Neurological Crisis: SCD Patient Presents with Fatal Extradural Hematoma
Author(s):
A 19 year-old patient presented with an isolated non-traumatic spontaneous epidural hematoma (EDH), an extremely rare consequence of sickle cell disease.
A recently published case report examined a young man with sickle cell disease (SCD) who experienced a rare and fatal neurological crisis.
Nearly 35% of individuals with the disease are affected by neurological manifestations including ischemic strokes, intra-parenchymal hemorrhage, and sub-arachnoid hemorrahage, sub-galeal hematoma, and extra-dural/epidural hematoma.
However, this 19 year-old patient presented with an isolated non-traumatic spontaneous epidural hematoma (EDH), an extremely rare consequence of sickle cell disease. Documented causes are associated with infectious disease, coagulation disorders linked with end-stage renal disease and hemodialysis, dural meastases, and Langerhans cell histiocytosis.
"Central nervous system problems are the most significant and morbid consequences of SCD," investigators wrote. "Extradural hematomas, in addition to infarction and hemorrhagic strokes, can develop in children with SCD. However, there is a scarcity of research detailing the prevalence and consequences of extradural hemorrhagic episodes in SCD, particularly in young adults."
Patient History
According to the report, led by Divit Shah, Department of Medicine, Jawaharlal Nehru Medical College, Datta meghe institute of medical sciences, the patient, from central India, was diagnosed with homozygous (HbSS) sickle cell disease at the age of 12 and a positive family history. He'd experienced multiple painful vaso-occlusive crises that resulted in hospital admission during his adolescence and underwent multiple blood transfusions.
At this time, he reported severe body ache and intermittent headaches over the course of 3 days. He was not taking hydroxyurea, but he was on symptomatic medical treatment (ibuprofen 400 mg intermittently and hydration).
Investigators noted that the patient had no prior co-morbidities like diabetes mellitus hypertension or tuberculosis, there was no history of gum bleeding or ecchymosis on the body, and he had denied any history of smoking and alcohol intake.
Clinical Intervention
Upon admission, the patient's pulse was 102 beats/minute with a regular rhythm, blood pressure 110/80 mmHg, respiratory rate 28/minute, with oxygen saturation of 96% on room air. The study reported that tachypnea was likely due to acute chest crisis, though his ABG (arterial blood gas analysis) was normal.
"On general examination, he was having icterus and mild, non-tender splenomegaly measuring 16 cms. Other systemic examinations were within normal limits. There was no sternal or bony tenderness," investigators wrote.
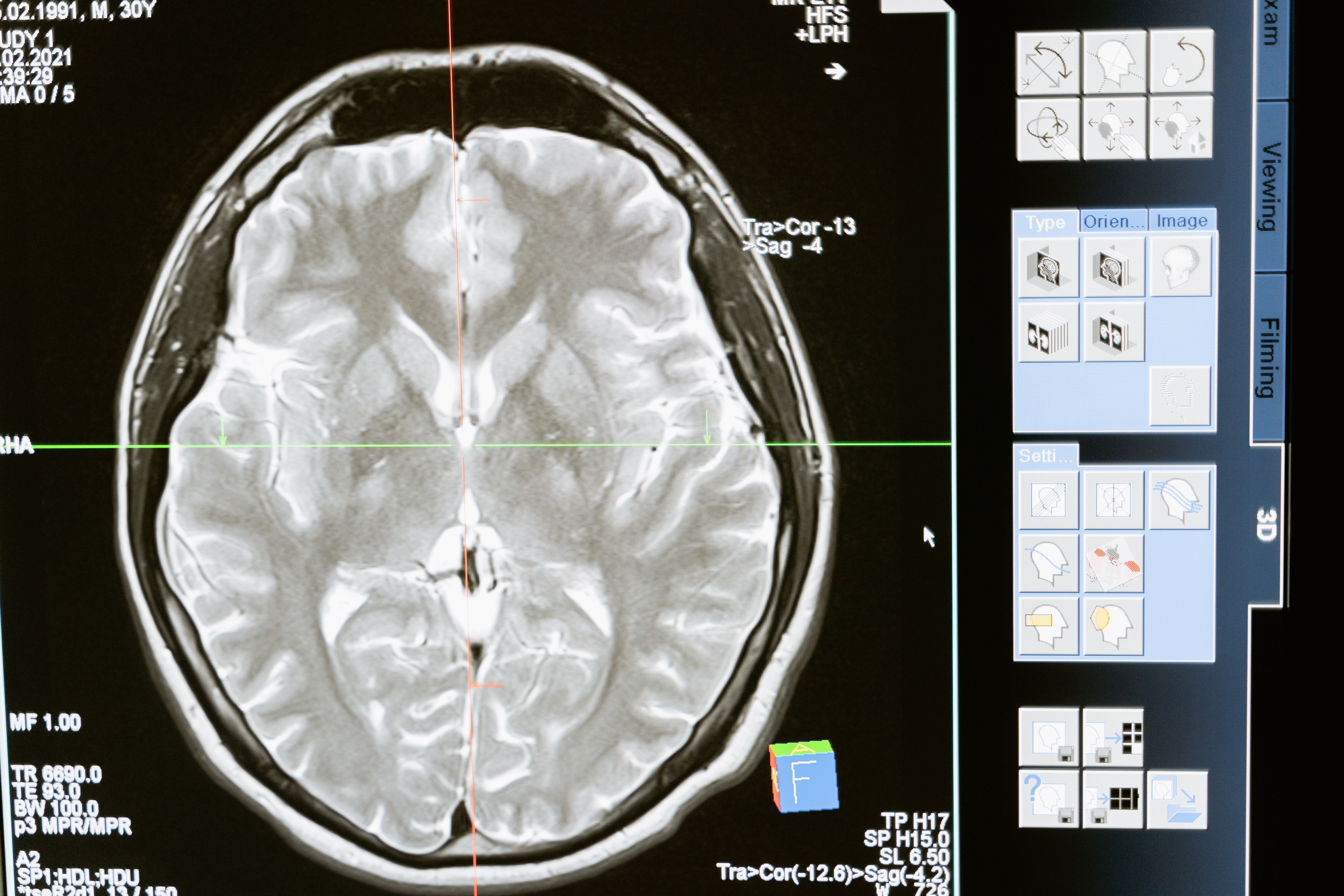
The patient was experiencing a severe headache and altered sensorium by the third day. A computerized tomography (CT) scan of the brain revealed the large extradural hematoma located in the right parietal region with mass effect and subfalcine herniation.
At this point, the patient was drowsy, his Glasgow Coma Scale (GCS) rose to 6 and was immediately intubated using a 7.5 mm endotracheal tube and attached to the ventilator. Physicians performed a transfusion of single-unit, single-donor platelet before emergency decompression surgery was initiated.
A significant decrease in the hematoma was revealed in a post-operative CT-brain scan 12 hours following the operation along with diffuse cerebral edema and in situ drain was placed subcutaneously.
Following the procedure, ventilatory support persisted and the physicians implemented nueroprotective strategies, mannitol, and broad-spectrum antimicrobial drugs until the patient succumbed, even after attempted resuscitation.
Cause Postulation
The long-term consequences can be especially severe for patients with an extradural hematoma and the rate of subsequent death is significant, according to the report. Therefore, investigators emphasized that suspicion of an EDH in a patient with sickle cell disease needs immediate neuroimgaging.
"The formation of extradural hematomas in SCD has been linked to unestablished pathophysiologies like vaso-occlusion of the hematopoietic calvarial diploic bone resulting in bone infarction and blood leaking into the periosteal, epidural, and sub-galeal regions," investigators noted.
Coagulopathy or platelet dysfunction can result in the development of a hematoma that leads to poor clinical outcomes.
"Acute and rapid increase in hematopoiesis, resulting in microfracture of the already thin inner cortex and blood and hematopoietic tissue extravasation with sludging of sickle cells in the diploic veins, obstructing venous drainage, and causing blood leaking due to vascular injury have also been postulated."
Investigators were unable to determine the cause of the patient's fatal spontaneous extradural hematoma, but speculated that it could have been instigated by bleeding due to his low platelet count (70,000/mm3).
While abnormal platelet counts are relatively common, previous research on patients with sickle cell disease found that acute chest syndrome with platelet count <200 × 109/L was an independent predictor of respiratory failure and neurologic complications, the report stated.
"Although vascular crisis is very common in SCD, an uncommon complication/crisis of sickle cell disease is a spontaneous extradural hematoma. When individuals appear with a sudden headache, it should be suspected. Although rare, extradural hematoma can be fatal and should be considered in patients with acute neurological symptoms," investigators concluded.
The study, "Sickle Cell Disease Presenting as Extradural Hematoma: An Extremely Rare Fatal Crisis" was published in Cureus.





