Article
Recurrent CDI Hospitalization in Patients with IBD May Not Increase Adverse Event Risk
Author(s):
Patients with ≥1 CDI-related admissions versus no CDI admissions experienced higher rates of 6-month readmission and annual cost across all hospitalizations.
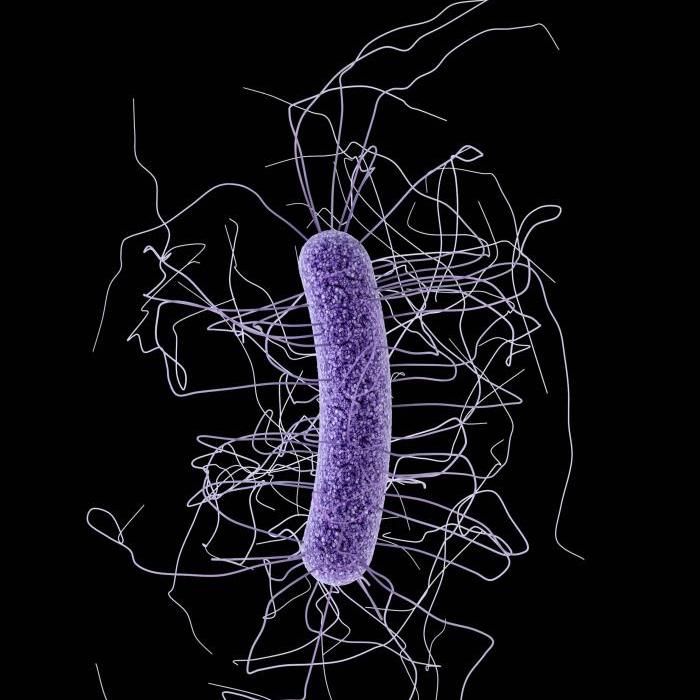
Although patients with inflammatory bowel disease (IBD) hospitalized for clostridiodes difficile infection (CDI) have poor longitudinal outcomes, new data suggest that recurrent admission for CDI may not increase the risk of adverse outcomes.
Study investigators noted it may be due to misclassification of CDI episodes, but more studies with a larger sample size is needed to examine the findings more closely and conduct adequately powered stratified analyses.
“A larger body of evidence examining long-term implications of rCDI hospitalization in IBD patients can inform how aggressively IBD specialists should pursue therapies to prevent rCDI, such as fecal microbiota transplantation in clinical practice,” wrote study author Preethi G. Venkat, MD, MPH, University of California, San Diego.
These findings were presented at the 2022 Digestive Disease Week Annual Meeting in San Diego, California.
Venkat and colleagues evaluated the impact of recurrent CDI-related hospitalization on longitudinal unplanned healthcare utilization in patients with IBD, using the Nationwide Readmissions Database 2017.
A total of 13,446 patients with IBD, hospitalized ≥2 times from January to June 2017 and followed through December 2017 were identified. From this population, 1,148 admissions were CDI-related.
Investigators compared the annual burden of hospitalization and IBD-related surgery in IBD patients with recurrent CDI admission versus single CDI-related admission in the primary analysis and those with ≥1 CDI-related admission versus no CDI-related admission (secondary analysis).
Over the 6-month follow-up period, patients with 1 or more CDI-related admissions versus no CDI admissions experienced higher rate of 6-month readmission (61.1% vs 55.7%; P <.001), time spent in the hospital (median, 26 days vs 21 days; P <.001), and annual cost across all hospitalizations ($212,524 vs $184,384, P < 0.01).
Further, these patients experienced higher rates of increased inpatient mortality (3.28% vs 1.81%; P = .011), rate of severe hospitalization (34.9% vs 30.4%; P = .016), and risk of readmission in the subsequent 6 months (adjusted hazard ratio [aHR], 1.16; 95% confidence interval [CI], 1.07 - 1.26) compared to patients with no CDI-related admissions.
However, data show no significant difference when comparing patients with single versus recurrent CDI-related admissions:
- rate of readmission (63% vs 64.3%; P = .8)
- annualized time spent in the hospital (27 days vs 27 days, P = .62)
- annualized cost across all hospitalizations ($223,296 vs $183,786, P = 0.23)
- inpatient mortality (4.04% vs 1.11%, P = .14)
- Severe hospitalization (35% vs 32.8%, P = .72)
- Risk of IBD-related surgery (5.83% vs 5%, P = .89)
The study, “Impact of Recurrent Hospitalization for Clostridiodes Difficile on Longitudinal Outcomes in Patients with Inflammatory Bowel Diseases,” was presented at DDW 2022.





