Article
Research Team Captures Distinct Phenotypes for Multiple Sclerosis Patients
Author(s):
While phenotypes of multiple sclerosis (MS) are well-established, there remains heterogeneity among patients that fit existing clinical definitions.
While phenotypes of multiple sclerosis (MS) are well-established, there remains heterogeneity among patients that fit existing clinical definitions.
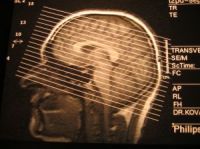
MRI-defined lesions and atrophy show only moderate inter-correlations, suggesting that they represent different disease processes in MS, at least in part. Now, studies are being conducted by several research groups to evaluate MRI-based categorization of cerebral lesions and atrophy in individual patients, in order to identify distinct MS phenotypes.
Shahamat Tauhid, MD, a research fellow at Harvard Institutes of Neurology at Brigham & Women's Hospital, in Boston, presented a poster at the Multiple Sclerosis: Advanced Imaging discussion session at the American Academy of Neurology (AAN) 2013 Annual Meeting describing one such study.
Tauhid and his colleagues studied a total of 175 MS patients with ages 42.7 ± 9.1 years and EDSS scores 2.5 ± 2.3. Within that population, 18 subjects had clinically-isolated syndrome (CIS), 115 were diagnosed with relapsing-remitting MS (RRMS) and 42 had secondary progressive MS (SPSS). Brain MRI measures included T2-hyperintense lesion volume (T2LV), the ratio of T1-hypointense LV (T1LV) to T2LV and brain parenchymal fraction (BPF). The median was used to create “bins” for each MRI parameter, with patients assigned a score of either low or high severity.
Four main phenotypes emerged from this analysis: Type I = low LV/mild atrophy (N=67; CIS=14, RR=47, SP=6); Type II = high LV/mild atrophy (N=21; RR=19, SP=2); Type III = low LV/high atrophy (N=21; CIS=4, RR=16, SP=1); and Type IV = high LV/high atrophy (N=66; RR=33, SP=33). Within each type, subgroups of “a” and “b” were defined by either a low or high proportion of T1LV.
To exemplify how MRI-based phenotyping relates to clinical observations, Tauhid reported the Type IVb phenotype — compared to Type 1a — showed higher EDSS scores (4.2 ± 2.4 versus 1.7 ± 2.1, respectively); different clinical subgroup composition (RR=21, SP=28) versus (CIS=9, RR=32, SP=6); and longer disease duration (14.7 ± 9.6 versus 6.0 ± 5.9 years). All parameters were significantly different for Type IVb compared to Type 1a (p<0.05).
Tauhid’s work indicates potential for utilizing MRI-categorization of lesions and atrophy to identify phenotypes in MS. Most patients have congruent extremes related to the degree of brain lesions and extent of atrophy. However, many other patients exhibit dissociation between lesions and atrophy, with one or the other feature being predominant.
Therefore, categorizations have been further refined by this research team in an attempt to capture all phenotypic variants that may have diagnostic and therapeutic utility. In addition, Tauhid and his colleagues anticipate that longitudinal studies will help define the uniqueness of these patterns and their clinical relevance regarding risk stratification and treatment response.



