Article
Researchers Highlight Studies on Pain Care for Wounded Veterans, Novel Treatments for Back Pain, and Neural Processes of Pain Modulation
Author(s):
The authors of three award-winning posters shared results and insights at the 2013 AAPM Annual Meeting.
Coordinated care to address the pain management and mental health care needs of severely injured military veterans, novel treatment approaches for low back pain, and identification of brain targets in chronic pain were the focus of a poster plenary session moderated by James C. Watson, MD, of the Mayo Clinic in Rochester, MN, at the 2013 American Academy of Pain Medicine annual meeting, being held April 12-14 in Fort Lauderdale, FL.
During the plenary session, Rollin M. Gallagher, MD, MPH, deputy national program director for pain management in the Department of Veterans Affairs and clinical professor of psychiatry and anesthesiology at the University of Pennsylvania and the Philadelphia VA Medical Center, provided insight into coordinated care efforts for service members with traumatic injury upon their return from service. In the Regional Analgesia Military Battlefield Pain Outcomes Study (RAMBPOS), the investigators evaluated 281 combat-injured military service personnel with major extremity injuries following initial acute-care hospitalization. The investigators evaluated pain parameters and improvements in health related quality of life (HRQOL) measures over a two-year period, every three months.
The investigators measured injury severity score (ISS) as well as other outcomes using the brief pain inventory (BPI), neuropathic pain scale (NPS), treatment outcomes in pain survey (TOPS), and VA Behavioral Health Laboratory. The investigators found that the most severe and critically injured patients had the most significant pain within the first three months; however, at six months, all patients had roughly the same pain level, suggesting the continued need for pain monitoring and management. In addition, over the two-year period, a number of patients developed problems readjusting socially at home and within the community. Many patients also experienced post-traumatic stress disorder (PSTD), which also suggests the continued need for effective long-term biobehavioral pain care.
Gallagher said that these results confirm that “chronic daily pain, including neuropathic pain, continues to be a burden for limb-injured servicemen, that post-traumatic stress is a far more prominent feature of recovery than in other chronic pain populations, and that returning to meaningful role functioning in their lives is challenging for many.”
Biologics for back pain
Also, during the session, Donald Myer, MD, PhD. of the Columbia Interventional Pain Center in Missouri, discussed the use of biologics in pain control for discongenic low back pain. Although using bone marrow aspirate concentrate (BMAC) is a controversial approach, the successes achieved in other applications convinced the researchers it may provide clinical benefit in this patient population. Myer presented retrospective data on 24 patients with low back pain with evidence of disc degeneration treated with BMAC over an 18-month period. Of the 24 patients treated, the investigators found that 12 patients required no further treatment and the other 12 required subsequent injection and/or surgical intervention.
While Myer was unable to provide insight into the patients who required subsequent treatment, those that required no further treatment were able to maintain limited pain over a two-year period, with most patients experiencing significant reductions in pain, improved activity tolerance, and reduced pain medication use. Overall, Meyer concluded that these findings support further prospective clinical trials evaluating the efficacy and safety of BMAC for discongenic low back pain.
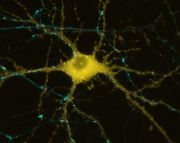
Neural processes underlying cognitive modulation of pain
In the final presentation of the session, Eric Dixon, BA, of Stanford University School of Medicine in San Francisco, CA, discussed neural correlates of effective cognitive modulation of acute pain. The investigators evaluated the successful cognitive modulation of pain in two studies, including a behavioral study, which identified adept modulators, and a functional magnetic resonance imaging (fMRI) study that determined neural correlates. During the behavioral study, the investigators identified 15 patients who were able to adeptly cognitively modulate their pain levels (ie, cognitively increase and decrease pain).
In the fMRI study, the investigators evaluated these 15 patients to identify potential neural correlates to cognitive pain modulation. The investigators found activation differences in areas related to pain processing, self-regulation, and cognitive control. Specifically, the investigators found the dorsal anterior cingulate (dACC) was activated during periods of increased and decreased pain, suggesting involvement of brain areas associated with pain processing and cognitive control. Dixon concluded that dACC may be a key component in modifying pain perception and should be further evaluated.





