Article
Gastrectomy Has More Favorable Long-Term Safety Outcomes Profile for Black, Hispanic Patients with Obesity
Karen Coleman, PhD

An analysis of data from more than 35,000 patients from 25 medical centers across the US details significant racial disparities in safety outcomes following bariatric surgery for Black and Hispanic patients undergoing Roux-en-Y gastric bypass (RYGB).
Using the National Patient-Centered Clinical Research Network (PCORnet) Bariatric Study, data from the present study indicate there was a low level of variability observed for weight loss and diabetes outcomes across racial and ethnic groups for both RYGB and sleeve gastrectomy, but point to clinically and statistically significant differences in safety and utilization outcomes for Black and Hispanic patients who had RYGB compared to sleeve gastrectomy, which investigators suggest could be indicative of differences in preoperative preparation and postoperative care processes rather than the procedures themselves.
“In this comparative effectiveness research study, findings suggest that the variability of comparative effectiveness of operations across racial and ethnic groups for percentage of total weight loss and HbA1c level was clinically small; however, differences for safety and utilization outcomes were both clinically and statistically significant for Black and Hispanic patients who had RYGB as compared with sleeve gastrectomy,” investigators wrote.
Led by Karen J. Coleman, PhD, of Kaiser Permanent Southern California, on behalf of the PCOR net Bariatric Study Collaborative, a team of investigators conducted the comparative effectiveness research study with the intent of bringing clarity to questions surrounding potential long-term differences in weight, diabetes, and safety and utilization outcomes among different forms of bariatric surgery based on a patient’s racial/ethnic background leveraging data from the PCORnet Bariatric Study. A retrospective observational comparative effectiveness cohort study, the PCORnet Bariatric Study was designed to capture accurate estimates of 1-, 3-, and 5-year benefits and risk of bariatric surgery. Launched in 2016, the study includes 25 health care systems across the US and provided investigators with data related to more than 60,000 patients.
Of the 60,000 patients included in the original PCORnet Bariatric study, 36,871 patients aged 12-79 years with a BMI of at least 35 kg/m2 who underwent a primary RYGB or sleeve gastrectomy from January 1, 2005-September 30, 2015, were included in the current study. The 36,871-patient cohort had a mean age of 45 (SD, 11.7) years and 19% were male patients. Investigators pointed out 19% were Black, 24% were Hispanic, 53% were White, 2% were recorded as other, and 2% had no recorded race or ethnicity. Investigators pointed 36,871 patients were included in the final analytic cohort for weight loss, 8407 were included in the final analytic cohort for type 2 diabetes outcomes, and 32,853 were included in the final analytic cohort for safety and utilization outcomes.
The study had multiple outcomes of interest related to weight loss, diabetes, and safety and utilization. The primary outcome of interest related to weight loss was the percentage of total weight loss. The diabetes outcomes of interest were type 2 diabetes remission, relapse, and change in HbA1c level. Safety and utilization outcomes of interest included operations, interventions, revisions/conversions, endoscopy, hospitalizations, mortality, 30-day major adverse events. All outcomes of interest were assessed 1, 3, and 5 years postprocedure.
Compared to their counterparts who underwent RYGB, those who underwent sleeve gastrectomy were younger (weight cohort, 44.1 years vs 45.7 years), with a lower BMI (weight cohort, 49.0 vs 49.8), and were more likely to be Black (weight cohort, 3963 vs 2898) and Hispanic (weight cohort, 4688 vs 4068). Compared with patients who had RYGB, patients who had SG also had a lower rate of many comorbid conditions at the time of surgery, including depression (weight cohort, 27% vs 33%), diabetes (weight cohort, 28% vs 44%), dyslipidemia (weight cohort, 45% vs 52%), eating disorders (weight cohort, 4% vs 18%), gastroesophageal reflux disease (weight cohort, 32% vs 45%), hypertension (weight cohort, 54% vs 64%), nonalcoholic fatty liver disease (weight cohort, 14% vs 26%), and sleep apnea (weight cohort, 40% vs 55%).
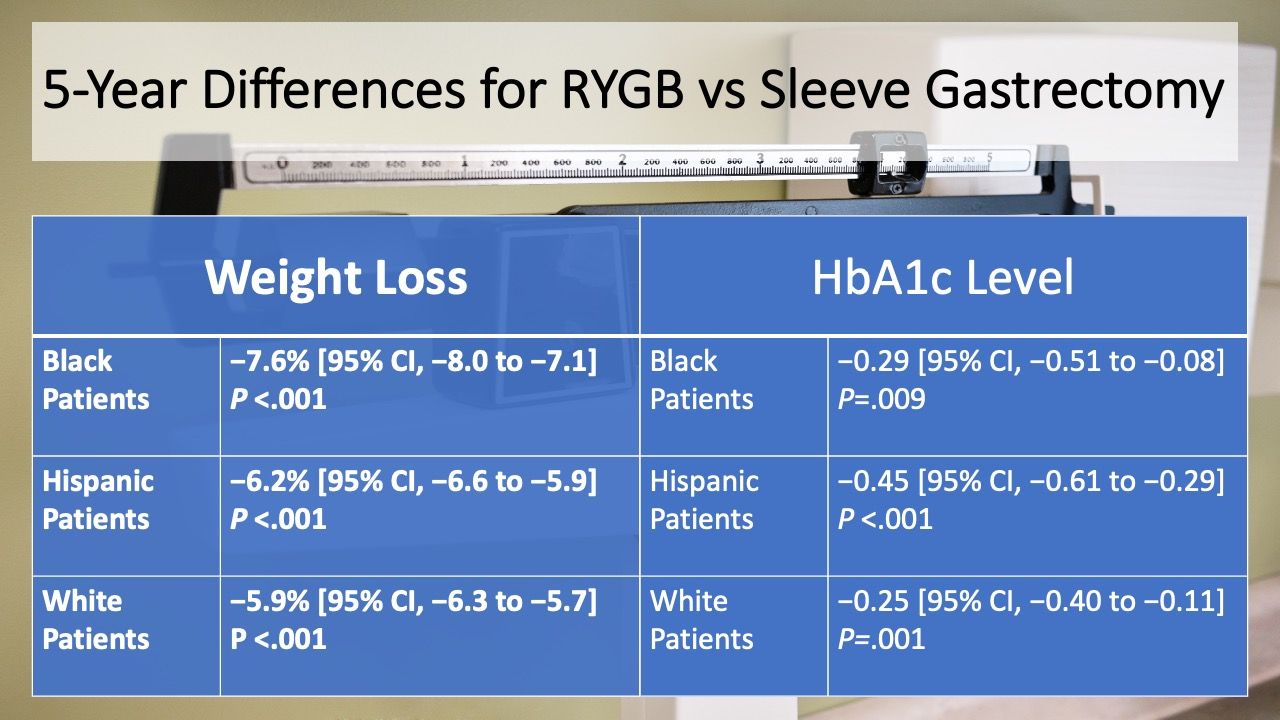
Weight loss and mean reductions in HbA1c level were larger for RYGB than SG in all years for Black, Hispanic, and White patients, with investigators noting the magnitude of difference among racial and ethnic groups for percentage of total weight loss being small. These differences are highlighted below.
Further analysis indicated Black (HR, 1.45 [95% 1.17 to 1.79]; P=.001) and Hispanic (HR, 1.48 [95% CI, 1.22 to 1.79]; P <.001) patients had a greater risk of hospitalization when they underwent RYGB compared to sleeve gastrectomy. Additionally, a greater risk of all-cause mortality (HR, 2.41 [95% CI, 1.24 to 4.70]; P=.01) and higher odds of a 30-day major adverse event (OR, 1.92 [95% CI, 1.38 to 2.68]; P <.001) was observed for Hispanic patients when undergoing RYGB compared to sleeve gastrectomy. Investigators pointed out no interaction between race and ethnicity with procedure type for diabetes remission and relapse.
In an invited commentary, Luise I. Pernar, MD, MHPE, Sherif Aly, MD, and Donald T. Hess, MD, all of the Department of Surgery at Boston Medical Center, detailed their reaction to the results, compared the data to that of other studies in the same arena, and noted where they felt immediate efforts might have the most benefit.
“It would be erroneous to argue in favor of sleeve gastrectomy for racial minority patients based on the less favorable safety profile of RYGB shown in this study. What the surgical community should strive for instead is to identify and eliminate the barriers to safe surgery for racial minority patients so they can benefit from the RYGB’s superior weight loss and improvement of obesity-associated medical conditions without the increased risk,” wrote the trio.
This study, “Comparative Safety and Effectiveness of Roux-en-Y Gastric Bypass and Sleeve Gastrectomy for Weight Loss and Type 2 Diabetes Across Race and Ethnicity in the PCORnet Bariatric Study Cohort,” was published in JAMA Surgery.



