Article
Shared Decision Making for Total Joint Replacement: The Physician’s Role
This surgery is an excellent option for relieving pain and restoring function in patients with osteoarthritis.
Initial treatment for patients who have osteoarthritis (OA)-a leading cause of pain and disability in the United States-may include diet, exercise, and NSAIDs. However, pain may persist despite conservative therapy. Total joint replacement (TJR) surgery is an excellent option for relieving the pain associated with OA and restoring functional status. Rates of patient satisfaction with TJR are high, although the total costs of hospitalization, physician reimbursement, and rehabilitation are on the order of $25,000 per case.1
When considering TJR, patients often turn to their physicians for guidance. The concept of shared decision making (SDM) has gained popularity in the medical community, especially for elective procedures such as TJR. SDM is predicated on open communication between the physician and patient. The physician provides comprehensive information about the procedure and its risks, benefits, and alternatives, and the patient informs the physician about personal, social, and cultural factors that may affect his or her decision-making process.2 In practice, however, physicians cannot expect that all patients will disclose or even be aware of the many elements influencing their decisions.
In this article, we address 10 questions that patients frequently ask when they are considering TJR. We also discuss social and cultural influences on patients' perspectives about TJR.
THE QUESTIONS
1. Is TJR right for me?
TJR is a good option for patients who experience severe pain or functional impairment resulting from hip or knee OA. Candidates for TJR generally are patients for whom conservative treatment with medications and physical therapy has not been successful. Because TJR is an elective procedure, patients often differ in the extent of functional limitation they will tolerate before proceeding with surgery. Therefore, specifying a threshold level of functional limitation required to proceed with TJR is not possible or appropriate. Specifying a pain threshold is also inappropriate. Patients may cite several factors, such as pain that disturbs sleep, pain on walking short distances, and unremitting pain, as reasons to proceed to TJR.
2. How will I benefit from TJR?
Most patients who undergo total knee replacement (TKR) or total hip replacement (THR) experience significant pain relief and improvement in function. Six months after TKR, 90% of patients report good or excellent outcomes.3 One year after TKR, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) function score increases by an average of 27.1 points, representing a dramatic improvement in functional status. Ten years after TKR, most patients experience either no pain or mild pain when they perform some activities and mild functional limitations during most activities4; 75% remain very satisfied with the results.5
Patients who undergo THR report similarly favorable outcomes. Eight years after THR, patients continue to report higher levels of physical functioning than before THR. These improvements are greatest among patients who had the most severe preoperative radiographic changes.6
3.What are the risks of TJR?
TJR is a safe procedure but, as with any operation, there are risks: 3.6% of patients who undergo TKR experience an adverse event within 90 days (eg, 1.5% have pneumonia, 0.9% have a myocardial infarction, and 0.9% have a pulmonary embolus). 7 Rates of deep venous thrombosis (DVT) can be as high as 88% in the absence of prophylaxis. However, use of either low-molecular weight heparin or oral coumadin in the postoperative period is now the standard of care; these agents have reduced the risk of symptomatic DVT to 1%.8
Some researchers also have promoted the use of a combination of modalities for DVT prophylaxis, including aspirin, mechanical compression devices, and early mobilization. For prevention of fatal pulmonary embolism, this multimodal approach seems comparable with other methods of chemoprophylaxis.9 Patients who have greater comorbidities or are older are at higher risk for perioperative adverse events.10 The mortality rate after TKR is 0.6%.7 The mortality rate is 30% higher for patients who undergo THR than for those who undergo TKR.10 Although the risk of death is higher immediately after surgery for patients undergoing THR compared with controls who do not have surgery, the risk diminishes greatly after 3 months and mortality is actually lower in those who had THR compared with those who did not. Some of this difference may be the result of selection bias, but the difference is not erased after adjusting for the higher rate of comorbidities in those who do not undergo surgery.11
4. Am I too old/young for TJR?
There is no upper or lower age limit for undergoing TJR. Because the prevalence of OA in older persons is high, TJRs are frequently performed in older patients. More than 50% of TKRs are performed in patients aged 70 years or older.12 In a study of 174 patients 65 years or older, patients were walking independently after a median of 12 days and were able to perform household chores after a median of 49 days.13 Patients who underwent TJR had significant improvements in physical function after 12 months compared with those who did not have TJR.
Although TJR is common in older patients, it is rare at the extremes of age. Among patients older than 100 years, the majority of THRs were nonelective procedures performed for fractures rather than elective procedures performed for OA. Post-TJR mortality was significantly higher in this population than in the general population.14
Comorbidities have a greater effect on functional outcome than does age. Patients who have at least 2 common geriatric problems (eg, falls, visual/hearing impairment, and balance problems) are 3 times more likely to have poor functional outcome than patients who have fewer than 2 such problems.15 In a study of 65 patients 90 years or older who underwent THR, 46% and 39% had medical complications after primary and revision THR, respectively. 16 None of the complications had long-term sequelae, and 96% of the patients were satisfied with the results of the THR.
Younger patients traditionally have not been offered TJR because of concerns about implant failure. Younger patients tend to be more active than older patients, leading to greater wear and tear of the joint replacements' bearing surfaces. In one study, only 83% of knee prostheses placed in patients 55 years or younger were still functioning 10 years after TKR, compared with 94% of knee prostheses placed in patients older than 70 years.17
Despite the lower rates of prosthesis survival in younger patients, 78% of knee prostheses are still functioning 20 years after TKR17 and 63% of hip prostheses implanted in patients younger than 50 years are functioning 25 to 30 years after THR.18 With growing recognition of the durability of prosthetic joints, the number of TKRs performed in patients aged 50 to 59 years increased 53.7% between 1990 and 2000.12 Prosthesis survival probably will increase further as new bearing surface technologies, such as highly crosslinked polyethylene, ceramic-on-ceramic articulations, and metal-on-metal coupling, are introduced and used more frequently.19
5. Should my weight affect my decision to have TJR?
TJRs often are performed in obese patients because obesity is a risk factor for hip and knee OA.20 Obese patients undergo THR an average of 10 years earlier than nonobese patients. Similarly, TKR is performed an average of 13 years earlier in obese patients compared with nonobese patients.21 The mean body mass index of patients undergoing TKR in the United States is 31.5 (normal range, 20 to 25).22 Because so many patients having TJR are obese, the effect of obesity on outcome is critical.
Studies have shown that overweight patients have worse functional outcomes after THR than their thinner counterparts.15 Overweight patients also have prolonged wound drainage23 and are more prone to dislocations.24 In addition, infections are more common in obese women undergoing TJR.
In spite of the increased risk of complications, overweight patients reap significant benefits from TJR. Five years after surgery, 70% of obese patients have good outcomes and 82% are satisfied with the results of surgery.24
6. What are alternatives to TJR?
Before undergoing TJR, patients should try conservative management with pain relievers, physical therapy, and weight loss.Some studies have shown improvement in walking speed and a decrease in disability after intra-articular hyaluronan therapy,25 but other studies have not consistently shown a benefit in pain reduction beyond that of placebo.26 For patients with unicompartmental knee OA, orthotic interventions (eg,valgus bracing and lateralwedged shoe insoles) may be effective options.
Arthroscopic procedures, such as debridement and lavage, often are performed but are largely ineffective for OA. The value of arthroscopic partial meniscectomy in patients with OA and concomitant symptomatic meniscal tear has not been established. In a landmark study that compared arthroscopic debridement/lavage with placebo surgery, patients who underwent arthroscopy did not have lower postoperative pain scores than those who had the placebo surgery. 27 This finding was confirmed by a recent randomized trial of 178 patients with knee OA that showed no difference in total WOMAC scores at 2 years follow-up between participants who had arthroscopic knee surgery and those who were managed with physical and medical therapy alone.28
Surgical treatments for patients who have unicompartmental knee arthritis include unicompartmental knee arthroplasty and osteotomy. The former is less invasive than TKR and is associated with faster rehabilitation time.The latter usually is performed in younger patients, especially in the presence of deformity, and has been shown to decrease pain and improve function. However, satisfaction rates are lower than those for TKR,29 and a recent cost-benefit analysis of unicompartmental knee arthroplasty versus TKR showed that TKR has significantly better long-term survival than unicompartmental knee arthroplasty.30
7. When should I have TJR?
Determining optimal timing for TJR requires consideration of several factors, including preoperative functional status. Historically,physicians often delayed surgery in patients with good functional status because early TJR was associated with an increased risk of prosthesis failure and a greater need for revision arthroplasty. However, prosthetic joints now have longer lifetimes. In addition, recent studies have shown that patients with better preoperative functional status have better postoperative functional outcomes.31-33 Patients who had lower preoperative pain scores also have less pain postoperatively than patients who had high preoperative pain scores.34 These findings suggest that considering TJR earlier in the course of disease may be appropriate.
To maximize preoperative functional status, some studies have examined the role of preoperative exercise on postoperative function and rehabilitation. Although postoperative functional status was similar regardless of preoperative exercise, participants who participated in a 6-week exercise program were 73% less likely to require inpatient rehabilitation.35
8. Where should I have TJR?
TJR is performed in a wide range of hospitals. Hospitals that have a high volume of TKRs (eg, more than 200 per year) have 25% fewer perioperative adverse events and 30% lower mortality rates than hospitals that have lower volumes.36 Rates of pneumonia and deep wound infection are significantly lower in high-volume hospitals than in low-volume hospitals.36 Two years after surgery, patients who underwent TKR in hospitals reporting more than 200 TKRs per year are less likely to have poor functional outcomes than those who underwent TKR in hospitals performing 1 to 10 TKRs annually.31 Preoperative teaching programs and dedicated orthopedic operating rooms also are associated with better outcomes after TKR.7
Volume is inversely associated with mortality and complications after THR. However, the association between hospital volume and patient-reported THR outcomes is not as clear.There is no association between hospital volume and functional outcome 3 years after THR, but satisfaction is higher in patients who underwent THR in high-volume hospitals than in those who underwent THR in low-volume hospitals.37
9. Who should perform my TJR?
Patients who undergo TJR performed by surgeons who do more than 50 TKRs per year are less likely to have medical complications36 and poor functional outcomes31 than patients who undergo TJR by surgeons who perform fewer than 13 TKRs per year. The best functional outcomes occur in patients who have had surgery done by high-volume surgeons in high-volume hospitals. Such a combination often is seen in the setting of an academic center, where residents and fellows may play an important role in the procedure. Surgeries performed by residents and fellows are associated with longer procedure times, but complication rates are similar between surgeries performed with trainee participation and those that do not involve residents and fellows.38
10. How long does it take to heal after TJR?
The average length of hospitalization for TKR is 4 to 5 days (Table); 51% and 58% of patients who underwent TKR12 and THR,39 respectively, were discharged to inpatient rehabilitation facilities. With the help of a physical therapist, most patients can attempt ambulation as soon as 1 day after surgery. However, only 23% of patients who underwent THR are able to walk independently at the time of hospital discharge39; they typically require a walker, crutches, or a cane to help ambulation.The highest rate of recovery occurs within the first 6 to 9 weeks after surgery. Physical therapy continues for several months. The total healing process may take 3 to 6 months.
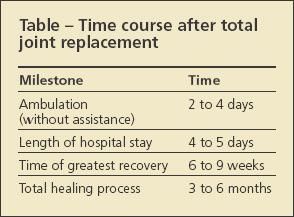
Table
SOCIAL AND CULTURAL FACTORS
By providing evidence-based answers to medical questions, physicians enable their patients to make informed decisions about TJR. These decisions are based on medical information as well as the personal values of physicians and their patients. These values are shaped by sex, race, and other social and cultural factors.
Several studies have assessed racial, ethnic, and sex disparities in TJR.40 Most of these studies have focused on differences in priorities and expectations between groups of patients. For example, women are less likely to undergo TJR than men. Focus groups have shown that women are more concerned than men about becoming a burden to their family after surgery.41 Therefore, they may place greater emphasis on healing time, length of hospitalization stay, and need for inpatient rehabilitation. They also may be more risk-averse.
Similarly, African Americans are less likely to have TJR than whites. Low rates of TJR among African Americans may be the result of a combination of low expectations for TJR and high expectations for alternative therapies. Many African Americans view prayer as a useful method of managing arthritis and, among those who believe in prayer, fewer view surgery as an acceptable alternative.42
Compared with white men who have OA, African American men with OA have lower expectations for the outcomes of TJR, independent of socioeconomic variables, literacy, and social support.43 Interventions such as an educational videotape and tailored decisionmaking may improve expectations among African American men,44 but it is not clear whether these interventions improve TJR rates.
These examples illustrate the complexity of decision making with regard to TJR and other elective procedures.The decision to undergo TJR requires comprehensive, effective communication between physician and patient via a shared decision-making process. Physicians must understand both the medical aspects of TJR and the social and cultural factors that influence their patients' preferences.
References:
References
- Chang RW, Pellisier JM, Hazen GB. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996;275:858-865.
- Whitney SN, McGuire AL, McCullough LB. A typology of shared decision making, informed consent, and simple consent. Ann Intern Med. 2004;140:54-59.
- Woolhead GM, Donovan JL, Dieppe PA. Outcomes of total knee replacement: a qualitative study. Rheumatology (Oxford). 2005;44:1032-1037.
- Wright RJ, Sledge CB, Poss R, et al. Patient-reported outcome and survivorship after Kinemax total knee arthroplasty. J Bone Joint Surg. 2004;86A:2464-2470.
- Miner AL, Lingard EA, Wright EA, et al; Kinemax Outcomes Group. Knee range of motion after total knee arthroplasty: how important is this as an outcome measure? J Arthroplasty. 2003;18:286-294.
- Cushnaghan J, Coggon D, Reading I, et al. Long-term outcome following total hip arthroplasty: a controlled longitudinal study. Arthritis Rheum. 2007;57:1375-1380.
- Solomon DH, Chibnik LB, Losina E, et al. Development of a preliminary index that predicts adverse events after total knee replacement. Arthritis Rheum. 2006;54:1536- 1542.
- Eikelboom JW, Quinlan DJ, Douketis JD. Extended-duration prophylaxis against venous thromboembolism after total hip or knee replacement: a meta-analysis of the randomised trials. Lancet. 2001;358:9-15.
- Lotke PA, Lonner JH. The benefit of aspirin chemoprophylaxis for thromboembolism after total knee arthroplasty. Clin Orthop Relat Res. 2006;452:175-180.
- Mahomed NN, Barrett J, Katz JN, et al. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg. 2005;87A:1222-1228.
- Barrett J, Losina E, Baron JA, et al. Survival following total hip replacement. J Bone Joint Surg. 2005;87A:1965-1971.
- Jain NB, Higgins LD, Ozumba D, et al. Trends in epidemiology of knee arthroplasty in the United States, 1990-2000. Arthritis Rheum. 2005;52:3928-3933.
- Hamel MB, Toth M, Legedza A, Rosen MP. Joint replacement surgery in elderly patients with severe osteoarthritis of the hip or knee: decision making, postoperative recovery, and clinical outcomes. Arch Intern Med. 2008;168:1430-1440.
- Krishnan E, Fries JF, Kwoh CK. Primary knee and hip arthroplasty among nonagenarians and centenarians in the United States. Arthritis Rheum. 2007;57:1038-1042.
- Bischoff-Ferrari HA, Lingard EA, Losina E, et al. Psychosocial and geriatric correlates of functional status after total hip replacement. Arthritis Rheum. 2004;51:829-835.
- Pagnano MW, McLamb LA, Trousdale RT. Primary and revision total hip arthroplasty for patients 90 years of age and older. Mayo Clin Proc. 2003;78:285-288.
- Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg. 2003;85A:259-265.
- Keener JD, Callaghan JJ, Goetz DD, et al. Twenty-five year results after Charnley total hip arthroplasty in patients less than fifty years old: a concise follow-up of a previous report. J Bone Joint Surg.2003;85A:1066-1072.
- Huo MH, Gilbert NF. What’s new in hip arthroplasty. J Bone Joint Surg. 2005;87A:2133-2146.
- Liu B, Balkwill A, Banks E, et al. Relationship of height, weight and body mass index to the risk of hip and knee replacements in middle-aged women. Rheumatology (Oxford). 2007;46:861-867.
- Changulani M, Kalairajah Y, Peel T, Field RE. The relationship between obesity and the age at which hip and knee replacement is undertaken. J Bone Joint Surg. 2008;90B:360-363.
- Lingard EA, Katz JN, Wright EA, Sledge CB; Kinemax Outcomes Group. Predicting the outcome of total knee arthroplasty. J Bone Joint Surg. 2004;86A:2179-2186.
- Patel VP, Walsh M, Sehgal B, et al. Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone Joint Surg. 2007;89A:33-38.
- Lübbeke A, Stern R, Garavaglia G, et al. Differences in outcomes of obese women and men undergoing primary total hip arthroplasty. Arthritis Rheum. 2007;57:327-334.
- Huang MH, Yang RC, Lee CL, et al. Preliminary results of integrated therapy for patients with knee osteoarthritis. Arthritis Rheum. 2005;53:812-820.
- Brandt KD, Smith GN Jr, Simon LS. Intraarticular injection of hyaluronan as treatment for knee osteoarthritis: what is the evidence? Arthritis Rheum. 2000;43:1192-1203.
- Moseley JB, O’Malley K, Petersen NJ, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81-88.
- Kirkley A, Birmingham TB, Litchfield RB, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359:1097-1107.
- Rinonapoli E, Mancini GB, Corvaglia A, Musiello S. Tibial osteotomy for varus gonarthrosis: a 10- to 21-year followup study. Clin Orthop Relat Res. 1998;353:185-193.
- Koskinen E, Eskelinen A, Paavolainen P, et al. Comparison of survival and cost-effectiveness between unicondylar arthroplasty and total knee arthroplasty in patients with primary osteoarthritis: a follow-up study of 50,493 knee replacements from the Finnish Arthroplasty Register. Acta Orthop. 2008;79:499-507.
- Katz JN, Mahomed NN, Baron JA, et al. Association of hospital and surgeon procedure volume with patientcentered outcomes of total knee replacement in a population- based cohort of patients age 65 years and older. Arthritis Rheum. 2007;56:568-574.
- Escobar A, Quintana JM, Bilbao A, et al. Effect of patient characteristics on reported outcomes after total knee replacement. Rheumatology (Oxford). 2007;46:112-119.
- Röder C, Staub LP, Eggli S, et al. Influence of preoperative functional status on outcome after total hip arthroplasty. J Bone Joint Surg. 2007;89A:11-17.
- Davis AM, Agnidis Z, Badley E, et al. Predictors of functional outcome two years following revision hip arthroplasty. J Bone Joint Surg. 2006;88A:685-691.
- Rooks DS, Huang J, Bierbaum BE, et al. Effect of preoperative exercise on measures of functional status in men and women undergoing total hip and knee arthroplasty. Arthritis Rheum. 2006;55:700-708.
- Katz JN, Barrett J, Mahomed NN, et al. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg. 2004;86A:1909-1916.
- Katz JN, Phillips CB, Baron JA, et al. Association of hospital and surgeon volume of total hip replacement with functional status and satisfaction three years following surgery. Arthritis Rheum. 2003;48:560-568.
- Woolson ST, Kang MN. A comparison of the results of total hip and knee arthroplasty performed on a teaching service or a private practice service. J Bone Joint Surg. 2007;89A:601-607.
- de Pablo P, Losina E, Phillips CB, et al. Determinants of discharge destination following elective total hip replacement. Arthritis Rheum. 2004;51:1009-1017.
- Kane RL, Wilt T, Suarez-Almazor ME, Fu SS. Disparities in total knee replacements: a review. Arthritis Rheum. 2007;57:562-567.
- Karlson EW, Daltroy LH, Liang MH, et al. Gender differences in patient preferences may underlie differential utilization of elective surgery. Am J Med. 1997;102:524-530.
- Ang DC, Ibrahim SA, Burant CJ, et al. Ethnic differences in the perception of prayer and consideration of joint arthroplasty. Med Care. 2002;40:471-476.
- Groeneveld PW, Kwoh CK, Mor MK, et al. Racial differences in expectations of joint replacement surgery outcomes. Arthritis Rheum. 2008;59:730-737.
- Weng HH, Kaplan RM, Boscardin WJ, et al. Development of a decision aid to address racial disparities in utilization of knee replacement surgery. Arthritis Rheum. 2007;57:568-575.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.




