Article
Special Considerations Needed for AMD Patients Undergoing Cataract Surgery
Author(s):
The clinical challenges presented by AMD during cataract surgery imply the need for special considerations and monitoring.
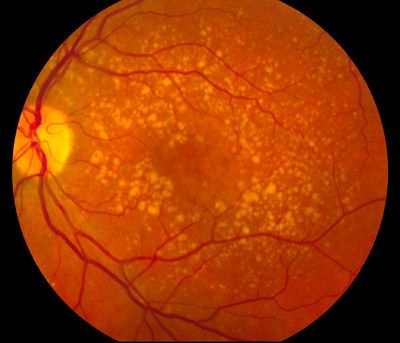
Special considerations should be taken when performing cataract surgery on patients with age-related macular degeneration (AMD) because patients with AMD pose specific challenges for surgery and recovery.
Boon Lin Teh, MBChB, with the Royal Infirmary of Edinburgh, served as the lead writer looking at the potential benefits and risks of cataract surgery associated with AMD and offered up a framework to assist clinicians in choosing "appropriate management" for their patients with cataracts and AMD.
Teh and colleagues claim that although cataract surgery is safe, commonly performed, and has led to increased benefits for patients in terms of function and visual acuity, patients with AMD "have a unique set of factors that have to be considered before deciding on surgery."
Clinicians and surgeons must determine whether the surgery will "benefit a patient with co-existing macular disease” and that the "risks of progression in AMD must be balanced against the potential for visual improvement," according to Teh. In order to weigh these factors, AMD patients require increased testing prior to surgery as part of a pre-operative workup, and throughout the post-surgical recovery.
Teh and colleagues suggested visual acuity, color vision, optical coherence tomography, optical coherence tomography angiography, and intravenous fluorescein angiography tests should be done. Additionally, Teh warns that the macula of patients with AMD may be more prone to developing "pseudophakic cystoid macular edema" which can further complicate cataract surgery for patients.
Teh stated that "the association between cataract surgery and AMD is a contentious one" and that many studies have determined cataract surgery as a risk factor for the development of AMD. The article points out that in 1998 a large-scale epidemiological study investigated the link between cataract surgery and increased risk of AMD, finding that patients with cataract surgery had a "significant increased risk of late AMD (43 of 869 eyes) and progression of AMD (209 of 6795 eyes)."
There is also, however, conflicting evidence from later studies suggesting that cataract surgery carries no significant increased risk for development of AMD. Teh and colleagues reviewed the available data and determined that currently, links between AMD and cataract surgery remain unsubstantiated and that further research is needed to confirm or deny any links.
Teh and colleagues also discuss the effects of anti-vascular endothelial growth factor (anti-VEGF) agents for treatment of AMD on cataract progression and surgery, stating that "cautious preoperative assessment is needed to anticipate and minimize any complications that might arise" because studies have shown a significant link between intravitreal anti-VEGF therapy and "increased risk of retained lens fragments after surgery and of both acute and delayed-onset endophthalmitis.”
The group recommended, due to the aqueous half-life of medications used in anti-VEGF therapy, that "cataract surgery should not preclude intravitreal injection if indicated," but should be left to the treating surgeon's "best clinical judgment" based on careful considerations of each individual patient's health and condition.
The article concluded that "maximizing vision-related life quality" for patients with cataracts and AMD will "inevitably require a bespoke plan encompassing elements of specialized optical, medical, surgical and low-vision rehabilitation care" and that purposeful testing, consideration, and monitoring are vital given the clinical challenges of performing cataract surgery on patients with AMD.
The article was published online and in the Survey of Ophthalmology.
Related Coverage
Subretinal AMD Therapy Improves Visual Acuity
Biomarkers Could Play Key Role in AMD Treatment, Detection
Unapproved Stem Cell Therapies Are Causing "Dismal" Health OutcomesUnapproved Stem Cell Therapies Are Causing "Dismal" Health Outcomes





