Article
Strict Treat-to-Target Approach Beneficial for Patients With RA
Author(s):
White a treat-to-target strategy is an important part of managing patients with rheumatoid arthritis, a more controlled implementation with closer follow-up appointments and patient education yielded better outcomes.
Patients with rheumatoid arthritis (RA) may benefit from a controlled treat-to-target (T2T), coupled with education and regular follow-up appointments, when compared with a casual T2T approach, according to a study published in Springer.1
“In addition to targeting clinical remission or low disease activity (LDA), close monitoring is also the keystone of T2T strategy implementation, which requires frequent visits to the clinic and good adherence to treatment,” investigators stated. “Insufficient adherence appears to be an important factor hampering the T2T implementation, resulting in increased disease activity and flares.”
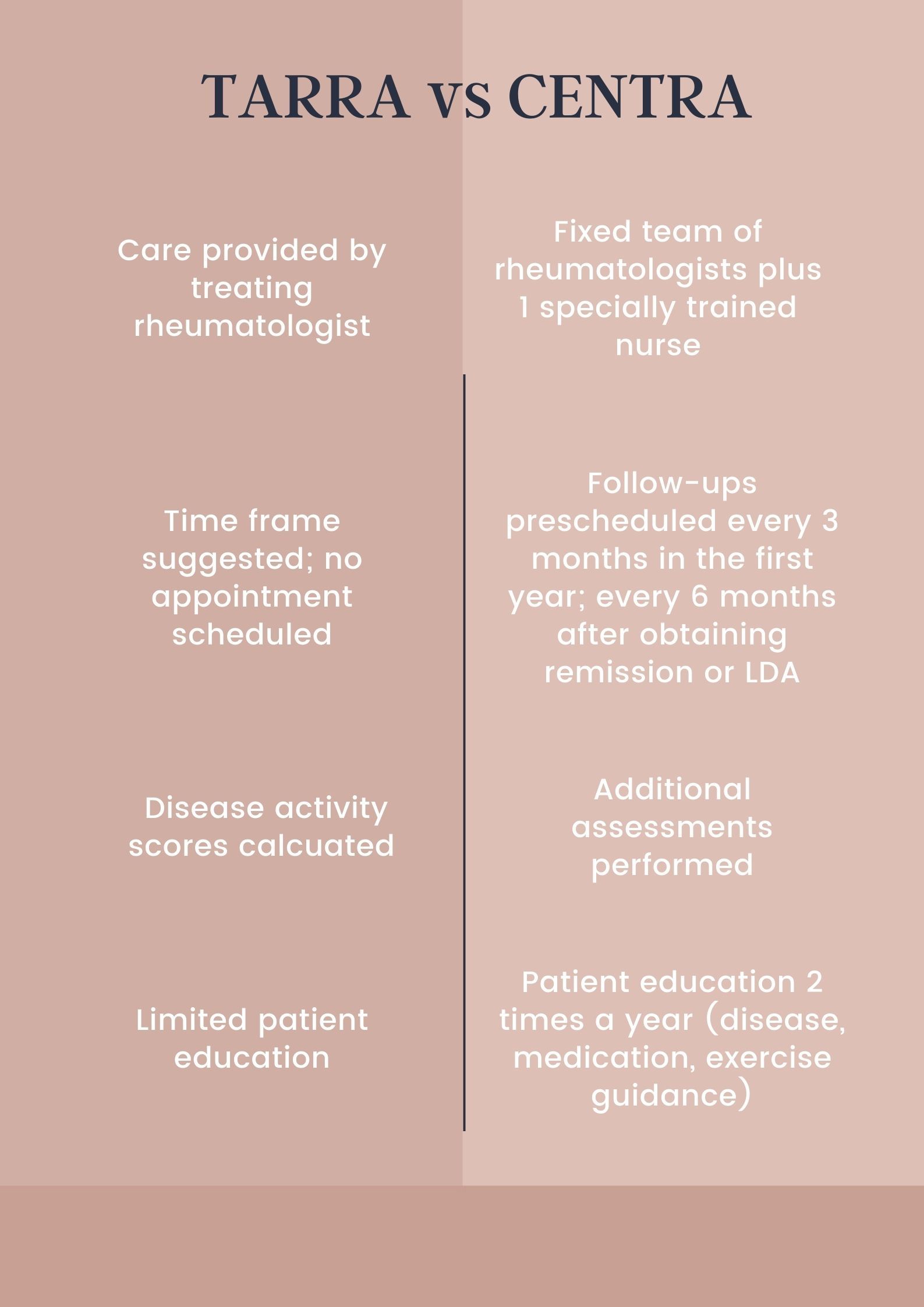
Investigators used data from the CENTRA (Collaboratively intENsive Treat-to-target in RA) and TARRA (Treat-to-TARget in RA) cohorts. TARRA, a longitudinal observational study, focused on casual control, while patients in CENTRA, a prospective cohort, followed a collaboratively tight-control T2T strategy. Patients in both cohorts were matched 1:3 by propensity score matching. The primary outcome was the Simplified Disease Activity Index (SDAI) at 1 year.
Patients in both groups had at least 3 follow-up visits with a minimum follow-up time of 1 year and were not absent for more than 12 months between appointments.
After an exclusionary process, 102 patients from CENTRA (enrolled between 2015 and 2019) and 271 patients from TARRA (enrolled between 2009 and 2015) were included in the analysis. Demographics, such as age and gender, disease course, and seropositivity were similar in both groups. While methotrexate (MTX) was used most often in both TARRA and CENTRA (81.2% vs 85.3%, respectively), a higher percentage of patients received glucocorticoids in the TARRA cohort (49.1% vs 24.5%, respectively).
Those in the CENTRA cohort had significantly lower SDAI scores when compared with the TARRA cohort (2.1 vs 3.4; p < 0.001). A generalized estimating equation (GEE) model yielded similar results (p = 0.0009) at the 1-year follow-up. Patients in the CENTRA group had better Clinical Disease Activity Index (CDAI) and Disease Activity Score based on 28 joints (DAS28) measurements at months 3, 6, and 24 when compared with the TARRA cohort. More patients in the CENTRA group were able to obtain SDAI-defined remission when compared with the TARRA cohort (72 [70.6%] vs 134 [49.4%]; p < 0.001).
The recruitment period varied in both studies, which limited the study as the evolution of disease may have been impacted by new medications available in addition to other factors. Prednisone doses were also higher in the TARRA cohort, however, T2T focuses more on strategy than medication and thus was not deemed an important influence. Radiographic and health assessment questionnaire data was not included in the study, as investigators analyzed disease activity and target achievement, which is associated with less joint damage, disability, and functional remission.
“Although T2T strategy has been ingrained into the management of patients with RA, the implementation still needs improvement,” investigators concluded. “Our study involving 2 cohorts of patients with RA with varied T2T implementations further corroborates the management of tight control with closer follow-up and appropriate education providing favorable outcomes.”
Reference:
Huang H, Xie W, Geng Y, et al. Towards a Better Implementation of Treat-to-Target Strategy in Rheumatoid Arthritis: A Comparison of Two Real-World Cohorts [published online ahead of print, 2022 Mar 28]. Rheumatol Ther. 2022;1-11. doi:10.1007/s40744-022-00441-0




