Article
Study Shows Some Positive Signs for Pancrelipase Against Non-Alcoholic Fatty Liver Disease
Author(s):
A new randomized controlled trial hints that pancrelipase may do better than conventional pancreatic enzyme supplementation in protecting against non-alcoholic fatty liver disease in pancreatic cancer patients who undergo pancreatoduodenectomy.
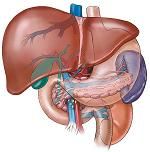
A new randomized controlled trial hints that pancrelipase may do better than conventional pancreatic enzyme supplementation in protecting against non-alcoholic fatty liver disease in pancreatic cancer patients who undergo pancreatoduodenectomy.
Pancrelipase patients developed non-alcoholic fatty liver disease at just over half the rate of control patients, but the observed differences in the small trial did not rise to the level of statistical significance.
Investigators randomized 29 such patients to pancrelipase and another 28 to a conventional pancreatic enzyme supplement. They checked for non-alcoholic fatty liver disease by looking for liver-to-spleen attenuation ratios of less than 0.9 on computerized tomography (CT) scans and by other measures from the clinic and the lab.
Overall, non-alcoholic fatty liver disease was observed in 6 of 29 pancrelipase patients (21%) and 11 of 28 control patients (39%). The investigators then switched 10 control group members who had developed non-alcoholic fatty liver disease to pancrelipase and observed improvement in 5 of those patients.
Multivariate analysis showed that advanced age and extended resection were independent risk factors for non-alcoholic fatty liver disease, but it did not differentiate between pancrelipase and the conventional pancreatic enzyme supplement.
“This randomized controlled trial did not show a significant protective effect of pancrelipase replacement therapy over conventional pancreatic enzyme supplementation on non-alcoholic fatty liver disease development after pancreatoduodenectomy for pancreatic cancer,” the investigators wrote in the Journal of Hepato-Biliary-Pancreatic Sciences. “Further studies are clearly required to investigate the etiology of and new therapeutic strategies for treatment-resistant non-alcoholic fatty liver disease.”
Prior studies have found strong evidence that pancrelipase does have some protective effect (compared to not treatment) against non-alcoholic fatty liver disease, which causes no symptoms or complications in many people but can cause inflammation and scarring in the liver.
A recent paper that appeared in the Journal of Hepato-Biliary-Pancreatic Sciences reported on 30 patients who developed non-alcoholic fatty liver disease after pancreaticoduodenectomy. Their mean liver-to-spleen CT ratio dropped from 1.233 before surgery to 0.453 when they were diagnosed with fatty liver disease. Treatment with pancrelipase increased the mean ratio to 0.762 after 1 month, 0.958 after 3 months and 0.904 after 6 months (p < 0.001).
“Mild liver dysfunction was also improved. Total protein, albumin and total cholesterol levels were significantly improved by the treatment. Importantly, relatively severe diarrhea seen in 11 patients was also ameliorated,” the study authors wrote. “Pancrelipase has a significant beneficial impact on non-alcoholic fatty liver disease after pancreaticoduodenectomy.”
Another study that appeared in the Journal of Gastroenterology followed 122 consecutive patients who underwent pancreaticoduodenectomy. The first 91 constituted the control group while the final 31 received high-titer pancrelipase and a solution rich in branch chain amino acids (BCAAs) via feeding tube, starting on the 4th day after surgery.
Investigators followed both groups— which had similar backgrounds, histopathology and operation-related variables — for 180 days after surgery and assessed them via CT scan and by measuring liver function and nutritional status.
“Liver attenuation and the liver-to-spleen attenuation ratio were significantly decreased, and the pancreatic parenchyma was significantly thinner in the control group at 3 months after the operation,” the investigators wrote. “The alanine aminotransferase levels were also higher in the control group (p < 0.05, at postoperative day [POD] 14, 30, 60 and 90), while the serum albumin (p < 0.05, at POD 30, 60 and 180) and total protein (p < 0.05, at POD 30, 60, 90 and 180) levels were significantly better in the pancrelipase-BCAA group.”




