Article
Surgery without instrumentation for spondylolisthesis-related stenosis?
Degenerative spondylolisthesis usually is asymptomatic but may be associated with symptomatic spinal stenosis. Because the latter often is detected by imaging studies in asymptomatic patients, clinical correlation between symptoms and imaging is critical.
ABSTRACT: Degenerative spondylolisthesis usually is asymptomatic but may be associated with symptomatic spinal stenosis. Because the latter often is detected by imaging studies in asymptomatic patients, clinical correlation between symptoms and imaging is critical. This patient presented with progressive exacerbation of symptoms of low back pain and leg weakness. An outpatient right endoscopic L4-5 laminotomy and foraminotomy was performed. After surgery, the patient reported complete resolution of his symptoms. Repeated flexion-extension x-ray films 16 months after the procedure showed no change in the degree of spondylolisthesis, and significant improvements were seen in outcome survey scores. We concluded that outpatient minimally invasive endoscopic decompression for spinal stenosis associated with degenerative spondylolisthesis is feasible. (J Musculoskel Med. 2011;28:125-136)
Degenerative spondylolisthesis, the slippage forward of one lumbar vertebra on another, rarely occurs in persons younger than 50 years and most often occurs at the L4-5 level.1 The condition generally is asymptomatic, but it may be associated with symptomatic spinal stenosis,2 the most common reason for lumbar surgery in persons older than 65 years.
Patients who have spinal stenosis, a narrowing of the spinal canal with compression of the neural structures, typically present with neurogenic claudication (pain in the buttocks or legs with walking or standing that resolves with sitting or lumbar flexion). However, spinal stenosis often is detected by imaging studies in asymptomatic patients; thus, clinical correlation between symptoms and imaging is critical.3
Several studies have compared surgical techniques for degenerative spondylolisthesis, but many of the studies involved instrumentation.4-6 In this case study, we assessed the feasibility and effectiveness of managing spondylolisthesis-related spinal stenosis via a minimally invasive outpatient approach that does not involve instrumentation. Our objective was to determine the optimal treatment strategy for patients with symptomatic degenerative spondylolisthesis.
Methods
Informed consent was obtained from the study participant. The patient underwent preoperative and 16-month postoperative flexion-extension imaging studies, which were reviewed for evidence of instability or progression of spondylolisthesis or both by independent radiologists blinded to the clinical results and unaffiliated with the operating institution.
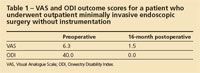
Similarly, the patient completed a preoperative and 16-month postoperative outcome survey that included the Visual Analogue Scale (VAS), 36-item Short-Form (SF-36) Health Survey Questionnaire, and Oswestry Disability Index (ODI). VAS scores range from 0 to 10 (lower scores indicate less severe symptoms), SF-36 scores range from 0 to 100 (higher scores indicate less severe symptoms), and ODI scores range from 0 to 100 (lower scores indicate less severe symptoms).

Case report
A 60-year-old man presented with progressive exacerbation of symptoms of low back pain and leg weakness. The symptoms had begun 5½ years before surgical treatment with a gradual onset of pain that worsened over time. The patient denied any injury or trauma when the pain started.
Associated symptoms included back pain, leg pain, buttock pain, leg weakness, and numbness and tingling, all bilateral. The patient stated that standing or walking aggravated the pain and sitting or lying down decreased it. The progressing pain and weakness had decreased his ability to exercise and greatly diminished his quality of life. Previous treatment included 6 to 8 weeks of physical therapy; there was no significant relief.

The patient’s primary care physician recommended MRI. Found at L4-5 were severe spinal stenosis (Figure 1) and grade 1 spondylolisthesis (Figure 2). The patient went to a local orthopedic surgeon and was offered an open posterior laminectomy and fusion at L4-5. He sought an alternative opinion, and his primary care physician referred him to another surgeon, who also recommended a fusion procedure.
The patient was hesitant to have major open back surgery and opted for an outpatient minimally invasive endoscopic surgery that did not involve hardware implantation. He underwent an outpatient right endoscopic L4-5 laminotomy and foraminotomy with thermal ablation of the facets bilaterally at L3-4, L5-S1, and the sacroiliac joints as well as left-sided facet ablation at L4-5.
The patient tolerated the procedure well. He was transferred to the recovery room via stretcher awake in stable condition and was released 2 hours postsurgery. There were no complications.
Results
The same day, after surgery, the patient was up and walking and reported complete resolution of his radicular pain, tingling, burning, and weakness. In addition, an independent review of repeated flexion-extension x-ray films showed no change in the degree of spondylolisthesis 16 months after the procedure. The patient reported that the back pain and leg weakness had not returned. He had been able to start exercising regularly and lost considerable weight.
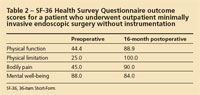
Significant VAS and ODI improvements were seen at 16 months postsurgery (Table 1). Similarly, significant improvements were seen in the patient’s SF-36 metrics for physical function, physical limitation, and bodily pain at 16 months postsurgery (Table 2). Although the mental well-being score decreased from 88.0 to 84.0, both of these numbers are above the mean and fall well within a standard deviation of the general US population.7,8
Discussion
Many authors have challenged the traditional treatment of patients with spinal stenosis in which wide laminectomy and facetectomy are performed with or without instrumentation.9-14 Although the goal of minimally invasive procedures without the use of instrumentation is to reduce postoperative pain and disability, the concern regarding the increased risk of postoperative spondylolisthesis remains.

The risk of spondylolisthesis has been regarded as a contraindication to decompression surgery, and many authors have suggested that concomitant fusion is indicated.6,9,15,16 In this patient, who underwent an outpatient right endoscopic L4-5 laminotomy and foraminotomy with facet ablation, increased instability did not occur, as demonstrated in the x-ray films (Figure 3), and there was complete resolution of his pain and disability, as demonstrated in his VAS, ODI, and SF-36 scores 16 months postsurgery.
Palmer and associates17 reported similar results. In their study, 8 consecutive patients with spinal stenosis and grade 1 spondylolisthesis underwent bilateral decompression via a similar minimally invasive outpatient approach. The mean preoperative VAS pain score was 7.6, and the average postoperative pain score was only 2.
Regarding facet ablation, numerous studies that involved such techniques as radiofrequency, laser, and cryodenervation reported rapid symptomatic relief; success rates range from 20% to 70%.18-24 Although there are published studies documenting efficacy, most studies are small and have limited follow-up. In addition, because peripheral nerves have the capacity to regenerate, we currently are evaluating the long-term outcomes.
Note that postoperative imaging was not performed in this case to verify decompression. Verification of the decompression of nerve roots and the spinal canal may be based on 2 sets of criteria, anatomical with imaging and clinical response. In our experience, because a disconnect may exist between symptoms and imaging, the clinical response demonstrated by relief of symptoms of neurogenic claudication is more relevant and provides sufficient evidence to indicate decompression, as was the case for this patient.
Ultimately, although decompression in conjunction with a fusion is the standard of care for lumbar degenerative spondylolisthesis, we contend that some patients may be treated with decompression alone. The criteria for endoscopic laminotomy and foraminotomy decompression without fusion in cases with same-level spondylolisthesis are the following:
•Symptoms related to neural compression.
•Conservative treatment has not been successful.
•Stable spondylolisthesis as determined by flexion and extension x-ray films.
•No previous surgery at said level.
Conclusion
Our results demonstrate the feasibility of performing outpatient minimally invasive endoscopic decompression for spinal stenosis associated with degenerative spondylolisthesis. The maintained stability that was observed in this patient may be the result of increased preservation of the normal ligamentous and muscular architecture with the minimally invasive procedure. Although this is only a single case study, the lack of increased instability validates investigation into a larger study, which we are pursuing.
References:
References
1. Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med. 2007;356:2257-2270.
2. Boden SD, Davis DO, Dina TS, et al. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects: a prospective investigation. J Bone Joint Surg. 1990;72A:403-408.
3. Atlas SJ, Deyo RA, Keller RB, et al. The Maine Lumbar Spine Study, Part III: 1-year outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine (Phila Pa 1976). 1996;21:1787-1794.
4. Bridwell KH, Sedgewick TA, O’Brien MF, et al. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord. 1993;6:461-472.
5. Fischgrund JS, Mackay M, Herkowitz HN, et al. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine (Phila Pa 1976). 1997;22:2807-2812.
6. Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg. 1991;73A:802-808.
7. Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey Manual and Interpretation Guide. Boston: New England Medical Center, The Health Institute; 1993.
8. Ware JE, Kosinski M, Keller SK. SF-36 Physical and Mental Health Summary Scales: A User’s Manual. Boston: The Health Institute; 1994.
9. Aryanpur J, Ducker T. Multilevel lumbar laminotomies: an alternative to laminectomy in the treatment of lumbar stenosis. Neurosurgery. 1990;26:429-432.
10. diPierro CG, Helm GA, Shaffrey CI, et al. Treatment of lumbar spinal stenosis by extensive unilateral decompression and contralateral autologous bone fusion: operative technique and results. J Neurosurg. 1996;84:166-173.
11. Nakai O, Ookawa A, Yamaura I. Long-term roentgenographic and functional changes in patients who were treated with wide fenestration for central lumbar stenosis. J Bone Joint Surg. 1991;73A:1184-1191.
12. Poletti CE. Central lumbar stenosis caused by ligamentum flavum: unilateral laminotomy for bilateral ligamentectomy: preliminary report of two cases. Neurosurgery. 1995;37:343-347.
13. Thomas NW, Rea GL, Pikul BK, et al. Quantitative outcome and radiographic comparisons between laminectomy and laminotomy in the treatment of acquired lumbar stenosis. Neurosurgery. 1997;41:567-574.
14. Young S, Veerapen R, O’Laoire SA. Relief of lumbar canal stenosis using multilevel subarticular fenestrations as an alternative to wide laminectomy: preliminary report. Neurosurgery. 1998;23:628-633.
15. Hopp E, Tsou PM. Postdecompression lumbar instability. Clin Orthop Relat Res. 1988;227:143-151.
16. Johnsson KE, Redlund-Johnell I, Udén A, Willner S. Preoperative and postoperative instability in lumbar stenosis. Spine (Phila Pa 1976). 1989;14:591-593.
17. Palmer S, Turner R, Palmer R. Bilateral decompressive surgery in lumbar spinal stenosis associated with spondylolisthesis: unilateral approach and use of a microscope and tubular retractor system. Neurosurg Focus. 2002;13:E4.
18. Cho J, Park YG, Chung SS. Percutaneous radiofrequency lumbar facet rhizotomy in mechanical low back pain syndrome. Stereotact Funct Neurosurg. 1997;68(1-4, pt 1):212-217.
19. Schaerer JP. Radiofrequency facet rhizotomy in the treatment of chronic neck and low back pain. Int Surg. 1978;63:53-59.
20. Iwatsuki K, Yoshimine T, Awazu K. Alternative denervation using laser irradiation in lumbar facet syndrome. Lasers Surg Med. 2007;39:225-229.
21. Li G, Patil C, Adler JR, et al. CyberKnife rhizotomy for facetogenic back pain: a pilot study. Neurosurg Focus. 2007;23:E2.
22. Koizuka S, Saito S, Kawauchi C, et al. Percutaneous radiofrequency lumbar facet rhizotomy guided by computed tomography fluoroscopy. J Anesth. 2005;19:167-169.
23. Savitz MH. Percutaneous radiofrequency rhizotomy of the lumbar facets: ten years’ experience. Mt Sinai J Med. 1991;58:177-178.
24. Staender M, Maerz U, Tonn JC, Steude U. Computerized tomography-guided kryorhizotomy in 76 patients with lumbar facet joint syndrome. J Neurosurg Spine. 2005;3:444-449.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.




