Article
tDCS Plus Mindfulness Meditation Practice Improved Quality of Life in Patients with Fibromyalgia
Author(s):
EULAR guidelines suggest that non-pharmacological therapies should be prioritized over treatment with medication.
Although repetitive anodal transcranial direct current stimulation (tDCS) plus mindfulness meditation (MM) did not improve pain or symptoms in patients with fibromyalgia syndrome (FMS), patients reported improvements in quality of life (QoL) when compared with the control groups, according to a study published in Fronteirs in Medicine.1 As the study had an underpowered sample size, future studies comprised of more participants coupled with longer follow-ups are needed to confirm results.
“FMS carries a large burden on patients owing to the cutbacks in daily life caused by chronic pain and associated symptoms such as sleep disturbances, fatigue, cognitive impairments and psychological problems,” investigators stated. “The most recent European League against Rheumatism guidelines recommend that once FMS diagnosis has been made, the primary focus should be on non-pharmacological therapies rather than treatment with medication. Thus, there is great interest in developing innovative non-pharmacological therapies to manage FMS pain and related symptoms.”
In the double-blinded, parallel, randomized, placebo-controlled pilot trial, investigators analyzed the clinical efficacy and feasibility of combining 2 non-pharmacological therapies (tDCS and MM) for pain and symptoms in patients with FMS. Patients were recruited through the outpatient pain clinic of the Department of Anesthesiology, University Medical Centre, Göttingen, as well as through advertisements, social media, patient support groups, and newspapers. Eligible patients were between 30 and 70 years old, met the American College of Rheumatology (ACR) Diagnostic Criteria 2010 for FMS, and had stable chronic pain for 6 or more months.
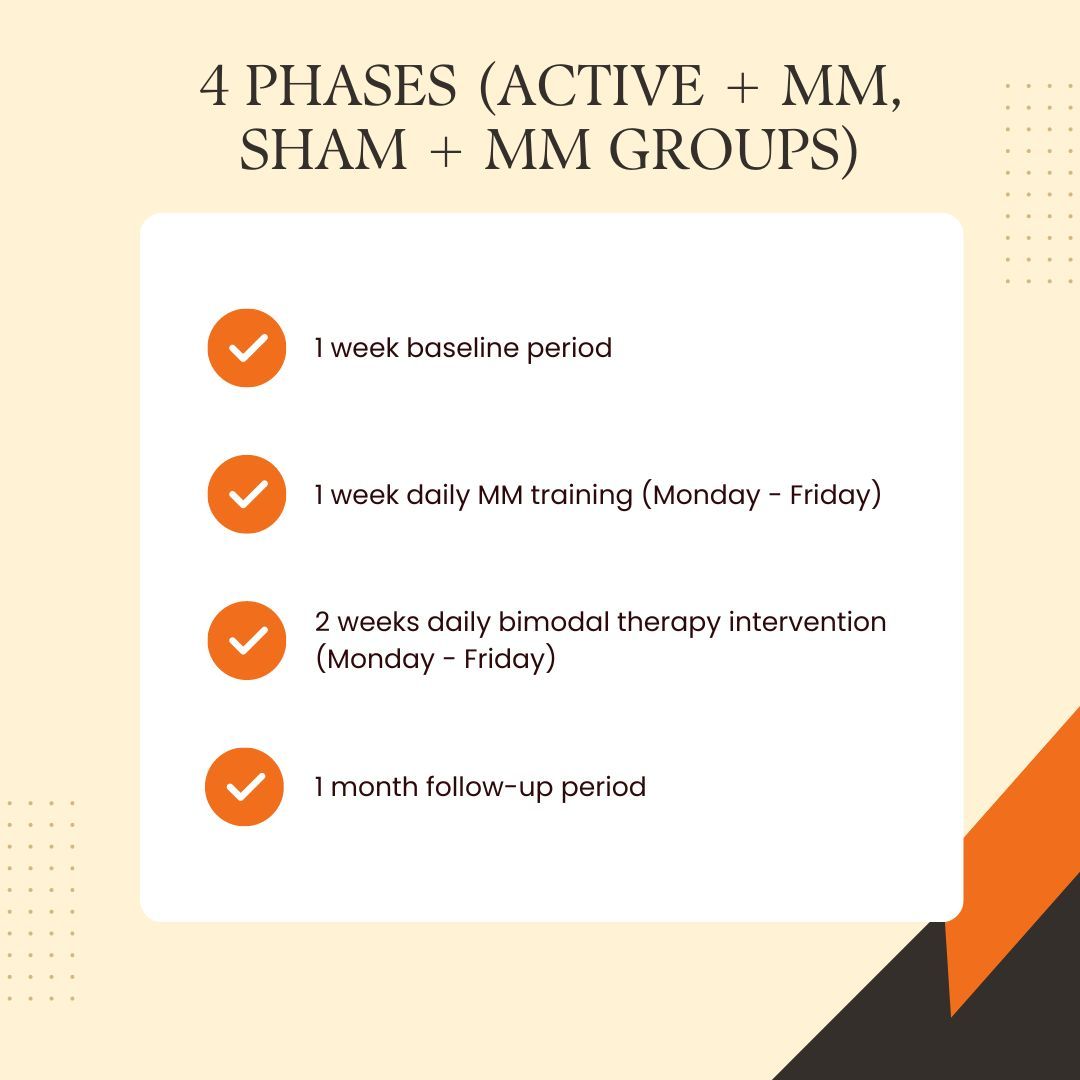
Patients were randomized to receive either 10 daily sessions of anodal tDCS over the left primary motor cortex coupled with MM for 20 minutes (active + MM, n = 10), sham tDCS combined with MM (sham + MM, n = 10), or no intervention (NoT, n = 10). Patients in the active + MM group and the sham + MM groups received MM training a week before the stimulation. Pain intensity was evaluated via a daily pain diary. QoL (Fibromyalgia Impact Questionnaire [FIQ]), pressure pain sensitivity (Pressure pain threshold [PPT]), sleep quality and quantity, and psychological wellbeing (Depression, Anxiety and Stress Scale- 21 Items [DASS]) were also assessed. Evaluations were performed at baseline, within 5 days after treatment, and 1-month follow up. Mindfulness was analyzed on the first and last day of MM training.
Thirty patients were included in the study. The mean age was 53.60 years, mean widespread pain index was 14.2, the mean symptom severity was 8.66, and nearly all participants were female (n = 28). Patients in the active + MM group did not experience reduced pain intensity when compared with controls, but they did report a clinically meaningful and significantly higher QoL. No significant difference across treatment arms was seen regarding psychological scales, pressure pain sensitivity, and sleep parameters. Treatment was well tolerated, and no serious adverse events were reported. The most common side effect was a light headache.
Including the training phase and the NoT group strengthened the study. However, the underpowered sample size hindered the quality of efficacy across treatment arms. Further, no monotherapy groups were included in the study, so investigators were not able to compare the intervention effects of tDCS and MM separately. Treatment administered in a group therapy setting may have led to non-specific psychological influences. As most patients were female and previous studies have indicated that different sexes perceive, modulate, and respond to treatment differently, future studies should address this factor.
“Still FMS patients in the active group reported clinically meaningful enhanced quality of life than those in the control groups immediately after the stimulation,” investigators concluded. “Future research with larger samples and extended follow-ups is required to further test the efficacy as well as to unravel the potential mechanisms underlying therapeutic effects of a combined MM and tDCS therapy.”
Reference:
Ramasawmy P, Khalid S, Petzke F, Antal A. Pain reduction in fibromyalgia syndrome through pairing transcranial direct current stimulation and mindfulness meditation: A randomized, double-blinded, sham-controlled pilot clinical trial. Front Med (Lausanne). 2022;9:908133. Published 2022 Oct 12. doi:10.3389/fmed.2022.908133




