Article
Why Telehealth Might Be Here to Stay in Psychiatry
Author(s):
Jesse Wright, MD, PhD, discusses the convenience of telehealth during the COVID-19 pandemic.
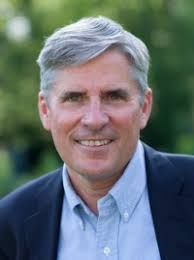
Jesse Wright, MD, PhD
The 2020 American Psychiatric Association (APA) Annual Meeting was cancelled this year, with plans made to convert the world-leading psychiatry conference into a two-part virtual session and educational platform for attendees.
In lieu of regular on-site coverage, HCPLive® will be running a series of interviews, insights, and reporting on topics that frequently headline the APA meeting—featuring familiar experts.
The coronavirus disease 2019 (COVID-19) pandemic has forced most psychiatry appointments to virtual platforms.
While there is an adjustment for both the patient and the clinician, many are seeing the value in utilizing new technology to streamline mental health more efficiently and safely.
In an interview with HCPLive®, Jesse Wright, MD, PhD, Director of the University of Louisville Depression Center, said while there are some hurdles that make care more difficult, many patients have spoken in favor of the convenience of telehealth in the last several weeks as face-to-face appointments were deemed unsafe.
Wright said thus far the majority of patients, some of which travel long distances and require to take off of work for appointments, have been impressed by the ease and convenience of telehealth and would prefer not to go back to traditional appointments.
However, for the patients dealing with more extreme issues, such as suicidal thoughts, telehealth may make things more difficult.
HCPLive: With COVID-19, is it more challenges to screen patients and develop these custom plans or is it in some way easier because they’re accessible and you know exactly where they are?
Wright: We’ve moved rapidly with telemedicine for our patients. I haven’t been in my office now for well over a month. And we seem to be going fine with treating patients using these techniques.
I think it’s working pretty well. There’s been research, by the way, that was done on telephone administered behavior therapy. It turned out that the outcome was the same as face-to-face therapy.
They actually favored telephone therapy a bit by having more people attend sessions. Many of the patients I’m contacting now by video like it a bunch. For example, a [patient] I just saw on video a few days ago usually has to drive a couple hours to come see me. He has to take a whole day off, drive a couple of hours, park, sit in the waiting room, have our visit, and then maybe have some lunch and drive back.
HCPLive: Does the fact that the pandemic is a global issue help a certain group of patients?
Wright: I’m sensing a much greater sense of community. Even though people are socially distancing and not attending in person church services or choir rehearsals or bowling leagues or baseball games, people are really making an effort to connect.
People are making an effort and I'm seeing that some of the patients that they'd like to begin to make an effort to reach out to them via video conferencing.
HCPLive: How do you think the COVID-19 pandemic has impacted the mental health of the country?
Wright: COVID-19 pandemic and crisis has hurt lots of people in a lot of ways, financially, their daily routine or rhythms are disrupted. We are going to see a jump in anxiety and depression. There haven’t been any statistics I’ve seen on that or formal studies done yet, but almost certainly you are going to find that there’s more of that out there. So, we have our work cut out for us in mental health.




