Article
Test Confirms If People Are Actually Taking PrEP to Prevent HIV
Author(s):
There are groups of people who are more likely to become infected with the human immunodeficiency virus (HIV) and, therefore, should be taking pre-exposure prophylaxis (PrEP). But are high-risk, HIV-negative people actually taking the preventive medication?
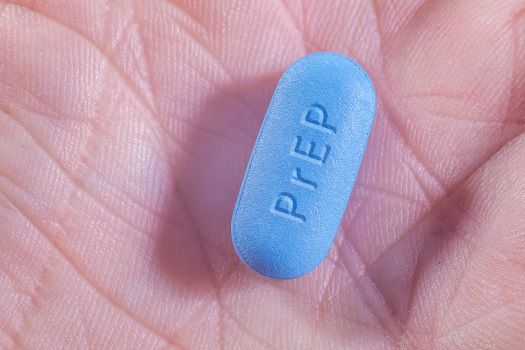
There are groups of people who are more likely to become infected with the human immunodeficiency virus (HIV), such as gay men, bisexual men, and people who inject drugs, and, therefore, should be taking pre-exposure prophylaxis (PrEP). But are high-risk, HIV-negative people actually taking the preventive medication? A new test, created by a team at the Skaggs School of Pharmacy and Pharmaceutical Sciences at the University of Colorado Anschutz, can answer that very question.
If used consistently, PrEP (branded under the name Truvada) can stop sexually transmitted HIV with 90% effectiveness. Lane Bushman, the lab manager at the CU Skaggs School of Pharmacy, developed an assay that can identify traces of antiretroviral drugs in just a spot of dried blood in order to see how much PrEP someone has been taking. Therefore, healthcare providers would be able to see if patients are in fact using the medication consistently.
- Related: Who Should Get PrEP and How to Reach Patients in Need
“There’s a need to objectively measure PrEP adherence because traditional ways have not been very effective,” Pete Anderson, PharmaD, a professor of pharmaceutical sciences at the CU Skaggs School of Pharmacy, said in a news release.
The assay works by putting a patient’s blood on an absorbent paper-like card. It is then sent to a lab in order to identify concentrations of PrEP drugs in the dried red blood cells.
“This assay takes advantage of the long half-life of PrEP medication in red blood cells. This means the drug builds up in these cells only if the patient takes it consistently,” Anderson continued. The test can estimate the number of PrEP doses someone has taken within the last month or two.
The researchers have already helped a lab in South Africa implement the method and it continues to be “in high demand for PrEP studies,” the CU statement said. The next step is finding a way to do the test bedside, which is already in motion with a recent grant given towards the cause.
It’s already being looked at if the assay can be used for other disease medications like hepatitis C. So not only could this method be implemented into most settings one day, but it may also apply to various conditions.
Also on MD Magazine >>> Major Gaps in HIV Research Leave Pregnant Women at Risk





