Article
Thai Study Identifies Predictive Factors behind Deadly Skin Disease
Author(s):
Among dermatologic conditions, necrotizing fasciitis (NF)-a potentially life-threatening infection of the skin and fascia-is notorious and nefarious. While it is not common in developed countries, NF has a high prevalence in undeveloped countries. Immediate treatment is essential, and thus, so is immediate and accurate diagnosis.
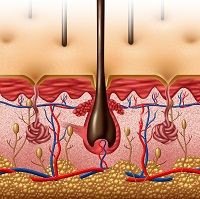
Among dermatologic conditions, necrotizing fasciitis (NF)—a potentially life-threatening infection of the skin and fascia—is notorious and nefarious. While it is not common in developed countries, NF has a high prevalence in undeveloped countries. Immediate treatment is essential, and thus, so is immediate and accurate diagnosis. For patients who contract NF, a new study published in Infection and Drug Resistance suggests some clinical characteristics that may be used to predict severe sepsis in NF patients.
Clinical presentation in early NF is tricky, because early signs are hard to detect; in fact, they can mirror simple cellulitis.Whenever the diagnosis and treatment are delayed or symptoms remain unidentified, postoperative morbidity or mortality will increase significantly.
The study was a retrospective observational cohort study. Almost 1,500 patients found to have NF by surgical or pathological confirmation were registered and treated at three Thailand hospitals from 2009 to 2012. The patient characteristics studied included sex, age, body mass index (BMI), education, occupation, underlying diseases, wound appearance, and site of wound. The study authors excluded all possible severe sepsis cases at admission to avoid incorporation bias.
Patients were divided in two groups: with and without severe sepsis. The study design was prognostic descriptive research with a retrospective cohort. Patients were categorized by demographic and clinical characteristics, and variables were compared between groups with and without severe sepsis. Then, a univariable analysis was carried out using a risk regression generalized linear model, with cluster hospitals used to identify the independent risk factors for severe sepsis. Third, clinically significant variables and statistically significant variables were included in a multivariable risk regression analysis, with generalized linear model cluster hospitals and step-backward method used to identify the independent risk factors for severe sepsis.
The study findings mirror and confirm earlier, small-sample-size studies that have shown that the risk factors for mortality and morbidity in NF patients. According to the study authors, “The clinical predictors for severe sepsis in patients with suspicion of NF included female sex, diabetes mellitus, chronic heart disease, hemorrhagic bleb, skin necrosis, and serum protein ,6 d/dL. The risk ratio was much higher in patients with total protein <6 g/dL, which is associated with malnutrition. Therefore, provision of sufficient nutritional support and close monitoring for these clinical predictors may be beneficial to reduce morbidity and mortality.”
The study also looked an antibiotic resistance, delay of surgical intervention after admission, and whether or not cases of gout can be associated with severe sepsis in NF patients. The study authors hope that awareness of these factors may reduce the incidence of severe sepsis in NF patients.




