Article
The 10 Best Health Stories from March 2017
Author(s):
The MD Magazine editors rounded up the 10 best stories from this month.

Conference coverage and approvals from the US Food and Drug Administration (FDA) were far from scarce this month. But the top 10 stories and videos from March consist of a wide variety of topics—including a post from the new feature section called First Person.
In case you missed it, our team covered the American Academy of Allergy, Asthma, and Immunology meeting (AAAAI 2017) in Atlanta, Georgia and American College of Cardiology meeting (ACC 2017) in Washington, District of Columbia. Keep an eye out because our team will be in San Diego, California covering the American College of Physicians Internal Medicine Meeting (ACP 2017) at the end of the month!
Don’t forget to stay up-to-date by connecting with MD Magazine on Facebook, Twitter, Instagram, and LinkedIn!
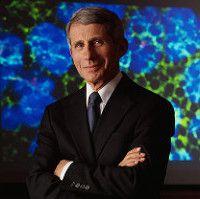
Editor’s Note: Anthony “Tony” Fauci, MD, has been the director of the National Institute of Allergy and Infectious Diseases (NIAID), since 1984, but to anyone who lived through it, his name will likely be forever linked to HIV and the progression to the early AIDS epidemic. Globally renowned for his research in immunology, Fauci also helped change the conversation of AIDS research at a time when AIDS patients and activists felt shunned by medical officials. Fauci was able to get the US Food and Drug Administration (FDA) to speed up their approval process to allow some drugs to be readily available. In recent years, Fauci has personally treated a patient afflicted with the Ebola virus. Fauci believes emerging infectious diseases will stay re-emerging, and plans to remain at the forefront of immunodeficiency research.
Fauci was a keynote speaker at the American Academy of Allergy, Asthma, and Immunology (AAAAI 2017) conference in Atlanta, Georgia, and spoke to MD Magazine in a video interview.
>>> Read the exclusive interview with Anthony Fauci, MD

Amy Scurlock, MD, of University of Arkansas for Medical Sciences & Arkansas Children’s Hospital, and colleagues conducted a study on long-term walnut oral immunotherapy (WOIT) and presented the findings at the annual meeting of the American Academy of Allergy, Asthma, and Immunology (AAAAI 2017) in Atlanta, Georgia.
Among the most common food allergens are the proteins found in cow’s milk, eggs, wheat, soy, fish, and shellfish. Peanuts and tree nuts—including walnuts, cashews, and pecans—are also common allergies, impacting around three million people in the United States, according to Food Allergy Research & Education. Allergies to nuts tend to last a lifetime, so identifying long-term treatment outcomes is crucial.
The aim of the research was to evaluate “the impact of long-term WOIT on desensitization and sustained unresponsiveness to both walnut and a test tree nut,” Scurlock explained.
>>> Continue reading this story here

Adding the PCSK9 inhibitor evolocumab (Repatha/Amgen) to statin therapy reduced by 15% the incidence of major adverse cardiovascular events in patients with vascular disease.
In a late-breaking clinical trial presented today at the American College of Cardiology Scientific Sessions (ACC 2017) in Washington, District of Columbia, a study known as FOURIER, researchers formally presented detailed results that elaborated on the basic findings already announced by Amgen.
A second study of the drug known as EBBINGHAUS, dealing with the drug’s impact on cognitive function in these patients will be presented at the meeting March 18.
>>> Continue reading this story

Physicians are ignoring guidelines on safe prescribing of opioids.
“The statistics are startling,” G. Caleb Alexander, MD, MS, an associate professor epidemiology at the Johns Hopkins Bloomberg School of Public Health (JHSPH), said in a news release in regards to a recent study conducted at the university.
Buprenorphine (Butrans/Purdue; others) is commonly used to treat opioid addiction. The prescription drug helps patients become less physically dependent on opioids and provides relatively mild withdrawal symptoms. In the journal Addiction, the JHSPH researchers reported that 2 in 5 people (43%) receiving buprenorphine are also receiving an opioid prescription.
>>> Continue reading this story

Editor’s note: In the new MDMag feature, First Person, physicians contribute creative writing, including poetry like this one from Diana Farid, MD, of Stanford University. She tells of trying to help a young patient who is unhappy in an arranged marriage to a much older man.
>>> Read this First Person feature story

Mark S. Forshag, MD, MHA, GSK, spoke with MD Magazine at AAAAI 2017 in Atlanta, Georgia, about the importance of eosinophils in treating severe asthma. Forshag said his team focused on the mass cell and have come to realize there are additional forms of inflammation mediated by the eosinophil cell.
Forshag also shared how phenotypes help identify patients that "are a little different from others". According to Forshag, learning the basis of phenotypes is necessary for understanding the use of the monoclonal antibody Nucala, which is directed against interleukin 5.
>>> Watch the exclusive interview with Mark S. Forshag, MD

A drug safety advisory committee joint panel today told the US Food and Drug Administration (FDA) to restrict or even end sales of oxymorphone hydrochloride extended release tablets (OpanaER/Endo Pharmaceuticals). The panelists were members of the Drug Safety and Risk Management Advisory Committee and the Anesthetic and Analgesic Drug Products Advisory Committee who met jointly.
Near the conclusion this afternoon of a two-day meeting, the group voted 18 to 8 with one abstention to reject the FDA’s current position that the benefits of the approved drug outweigh its risks.
Voting “no” meant the committee members were advising the FDA to take some remedial action. Choices range from taking the drug off the market, requiring physicians to get more education on how to prescribe the drug, adding a “black box” warning to its label about its potential to be abused, or other measures.
>>> Continue reading this story
Just after heart attack and stroke, venous thromboembolism (VTE) is the third leading vascular diagnosis. The condition impacts hundreds of thousands of Americans every year. While there are treatments for the two types (deep vein thrombosis (DVT) and pulmonary embolism (PE)), the condition remains serious and life-threatening.
Paul Burton, MD, PhD, vice president of Medical Affairs at Janssen, filled MD Magazine in on the phase 3 EINSTEIN CHOICE trial results at the 66th Scientific Session of the American College of Cardiology (ACC 2017) in Washington, District of Columbia. The trial examined the use of rivaroxaban (Xarelto/Janssen) or aspirin as extended treatment in patients with VTE.
>>> Watch the exclusive interview with Paul Burton, MD, PhD

Based on the work of “the largest Task Force ever convened for the development of EULAR recommendations,” the European League Against Rheumatism has compiled a meticulous update of their previous recommendations for the management of rheumatoid arthritis (RA), which includes several changes from previous 2010 and 2013 guidelines.
Recently updated this March and published in Annals of the Rheumatic Diseases, EULAR’s own journal, the 2016 recommendations included input from rheumatologists from 14 European countries, as well as experts from North America, Asia, Latin America and Australia, in addition to three patients, for a total of 50 participants. The effort was led by Josef S. Smolen, MD, of the Medical University of Vienna in Austria, himself a former president of EULAR. The process of compiling the report, according to Smolen, took about a year, and features an extensive, separately-published literature review.
>>> Continue reading this story
For decades, science has attempted to nail down an answer as to whether the use of stimulant medications for the treatment of childhood attention-deficit/hyperactivity disorder (ADHD) can inhibit long-term growth. A recently-published study featuring a long-term follow-up falls on the side of the “yes, they can” argument.
The Multimodal Treatment Study of Children with attention-deficit/hyperactivity disorder (known as MTA) began in 1994 and continued straight through to 2013, and serves as the basis for the new report. With follow-up into adulthood at an average age of 25 years old at completion, the study was able to look at years’ worth of data and divide subjects into groups based on their adherence to ADHD medications. The study began as a 14-month randomized clinical trial to test medication management (Med), behavior modification (Beh), a combination of the two (Comb), or a treat-as-usual course for community comparison (CC) as possible routes for management of the condition.





