Article
Three-Drug Combo Prolongs HIV Treatment Effects
Author(s):
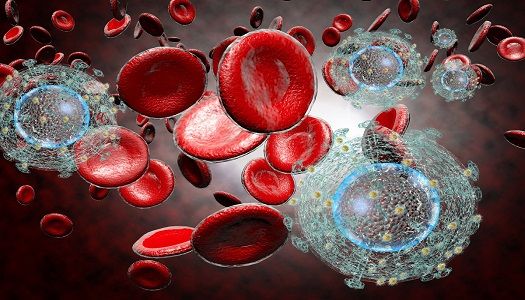
A novel drug extends the effects of already FDA-approved HIV drugs.
Physicians from the University of Rochester Medical Center (URMC) in New York developed a drug which extends treatment effectiveness against the human immunodeficiency virus (HIV).
The novel drug, appropriately named URMC-099, encourages cells to release their protective machinery to fight the virus. With fine-tuning, the researchers say that the drug can make it so patients’ daily antiretroviral therapy (ART) is only needed once or twice a year.
But how does URMC-099 help make such a drastic cut? The team had previously developed and tested the “nanoformulated” versions of two common ART drugs—a protease inhibitor (atazanavir) and an integrase inhibitor (dolutegravir), both of which have been approved by the US Food and Drug Administration (FDA).
These nanoformulated drugs were made with LASER ART (long-acting slow effective release antiretroviral therapy), a novel process which turns the drugs into crystals—which are protected from being destroyed by the liver and kidney elements. LASER ART allows the crystals to be taken to macrophages, immune system cells, in order to reach tissues and reside there for substantial periods of time.
When atazanavir, dolutegravir, and URMC-099 were combined, it was found that the process of autophagy can actually take place. Autophagy works by allowing cells to get rid of invading viruses and other intracellular “trash.” However, when HIV enters the picture, it stops the activation of autophagy—yet another reason why there isn’t a cure for the virus. When URMC-099 was introduced with the nanoformulated ART, cells are able to fight HIV even after treatment—therefore, extending virus-free time.
As described in The Journal of Clinical Investigation, the three drug combination was tested in human immune cells as well as mice that were modified to have a human immune system and HIV. URMC-099 did not have an antiviral effect on its own, but when combined with the two ART drugs, it lifted the autophagy block and inhibited viral growth.
In the animal model, this also led to a 50-fold increase in the plasma drug concentration of the viral dolutegravir. The reason for this, however, is unclear. The researchers plan to explore that question further.

“This study shows that URMC-099 has the potential to reduce the frequency of HIV therapy, which would eliminate the burden of daily treatment, greatly increase compliance, and help people better manage the disease,” Harris Gelbard, MD, PhD, professor and director of the University of Rochester’s Center for Neural Development and Disease, (pictured left) said in a news release.
While more research is needed, the researchers said the finding is a step towards long-acting anti-HIV drugs.
The study, “Autophagy facilitates macrophage depots of sustained-release nanoformulated antiretroviral drugs,” was published in The Journal of Clinical Investigation. The news release and headshot were provided by URMC.
Related Coverage:
Elite Controller’s Antibodies Combined to Defeat HIV
How HIV Gets the Opportunity to Infect Macrophages
CD4 Cell Count May Indicate COPD Risk in HIV-Positive Patients





