Article
Trajectories of Depression and Anxiety Among Patients with Systemic Lupus Erythematosus
More than 50% of patients with classified SLE at Washington University’s Lupus Clinic exhibit clinically meaningful and persistent depression and anxiety symptoms over time.
Mood disorders are a common and significant comorbidity among patients with systemic lupus erythematosus (SLE). It is estimated that up to 30% of patients exhibit comorbid depression and up to 37% experience anxiety. Since the American College of Rheumatology (ACR) updated its criteria to recognize neuropsychiatric manifestations of SLE in 1999, understanding the ways in which mood disorders impact patients with SLE has become extremely relevant. Further, determining whether mood disorders are a direct physiologic cause of SLE can help inform treatment for these patients.
Studies that have begun to evaluate the relationship between SLE disease activity and mood disorders have yielded mixed results. Additionally, much of the research examining prevalence of mood disorders among patients with SLE and their relationship with disease activity has been limited by cross-sectional study designs and small sample sizes. Given this context, we sought to examine the longitudinal course of depression and anxiety, and their relationship with SLE disease activity, among patients receiving care at Washington University’s Lupus Clinic.
This study took place in Washington University School of Medicine’s Lupus Clinic. This clinic exists to expand and improve care for patients living with SLE. Our sample included 144 patients with ACR or Systemic Lupus International Collaborating Clinics (SLICC)-classified SLE. Of this cohort, over half (56%) were Black while 40% were White. This uniquely situated our research, as Black participants are often underrepresented in studies of individuals with SLE, even though it is known that SLE disproportionately affects Black women. The most prevalent comorbidity in the cohort was hypertension, affecting about 40% of participants, and just under a quarter of individuals were on a prednisone dose greater than 7.5 mg/day at baseline. At each clinic visit, depression [Center for Epidemiologic Studies Depression Scale- Revised (CESD-R)], anxiety [Patient-Reported Outcomes Measurement Information System (PROMIS) Emotional Distress: Anxiety Short Form 8a], and SLE Disease Activity Index 2000 Responder Index-50 (S2K RI-50) scores were measured. Individuals with a minimum of three clinic visits over an average time of 30 months were included in the sample.
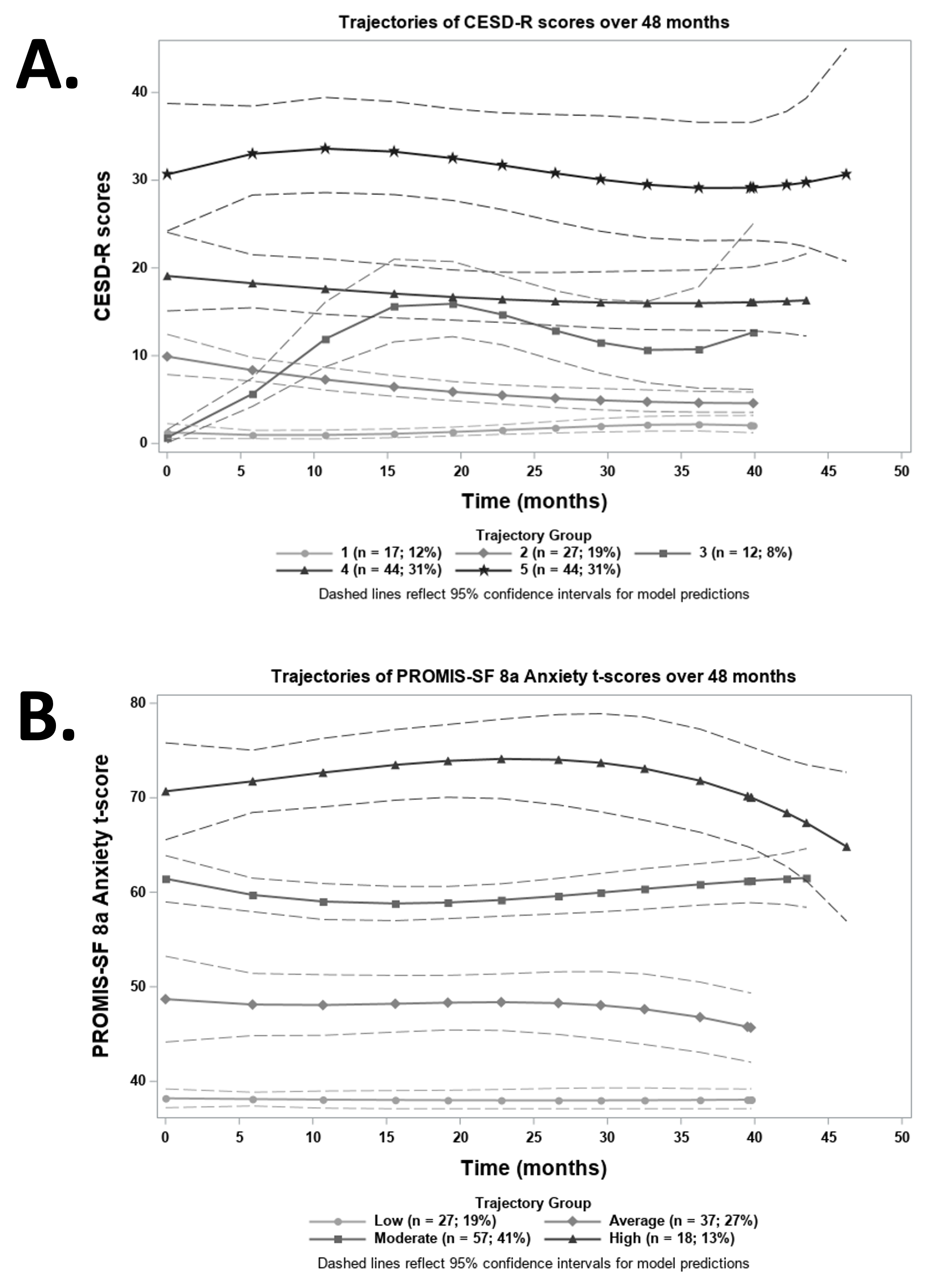
Depression and anxiety were both found to persist over time in more than half of the patients in the cohort. Group based trajectory modeling (GBTM) was performed, identifying 5 unique groups of patients with similar trends of depression over time (Figure 1A) and 4 unique groups of patients with similar trends of anxiety over time (Figure 1B). As can be seen from the figure, both depression and anxiety remained stable over time (Figure 1). Of note, there was a higher proportion of Black participants among the groups with the most severe symptoms for both depression and anxiety.
We further examined the relationships between both categories of mental health symptoms and disease activity over time using linear mixed models. Active SLE disease (represented by a S2K RI-50 score greater than 4) was significantly associated with depression symptomology, even after controlling for significant covariates of race and prednisone dose. In contrast, active SLE disease was not significantly associated with anxiety symptomology after controlling for significant covariates of race and CESD-R scores. Notably, race was associated with both depression and anxiety in these models, with Black patients having significantly higher levels of both mental health symptoms over time, compared with White patients.
Taken together, this work emphasizes that despite patients being established in care for their SLE disease, many individuals still exhibit high and persistent levels of depression and anxiety without noted improvement over time. This highlights the missed opportunities related to providing adequate mental health treatment for patients with SLE. It has recently proposed that SLE symptoms can be separated into two categories. While Type 1 symptoms are clinical findings, such as nephritis or cutaneous rash, Type 2 manifestations are subjective symptoms that are harder to measure, including fatigue, body pain, depression, or anxiety. In contrast with Type 1 symptoms, these Type 2 manifestations are not necessarily associated with periods of disease activity. Our findings support this distinction of Type 2 manifestations of SLE, showing inconsistent relationships between SLE disease activity and severity of mood disorders over time.
Moving forward, it is vital that we practically address the persistent nature of depression and anxiety noted in this cohort of patients with SLE. Access to adequate mental health care and services is clearly one of the areas to be addressed. Additionally, we are working to collect Social Determinants of Health (SDOH) to better understand the complex barriers facing patients with SLE and other rheumatic diseases. We are interested in further gathering information about patients’ financial stability, transportation needs, stress, social connections, and other domains of SDOH. In partnership with a clinical social worker, we are working to expand the social services team in our rheumatology clinics to ensure that patients receive direct access to referrals for reported mental distress or social needs. This will ensure that patients receive needed resources in a timely fashion. Ultimately, we will work to improve patients’ mental health by connecting them with both mental health services and resources for addressing social barriers that may be contributing to depression and anxiety.
For further details about this research, readers are encouraged to refer to our 2 recently published manuscripts: Depressed Symptomatology Persists Over Time in Systemic Lupus Erythematosus Patients and Anxiety Symptoms Among Patients With Systemic Lupus Erythematosus Persist Over Time and Are Independent of SLE Disease Activity
Figure 1. Identified trajectories of depression (A) and anxiety (B) scores over time