Article
Upadacitinib Better than Adalimumab in Rheumatoid Arthritis
Author(s):
A new study of AbbVie’s original JAK1-selective inhibitor indicates that it outdoes adalimumab without sacrificing safety in rheumatoid arthritis treatment.
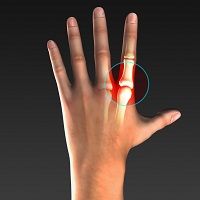
Upadacitinib (UPA)—an investigative, small-molecule, oral JAK1-selective inhibitor—proved superior to adalimumab (ADA) or a placebo (PBO) in inhibiting rheumatoid arthritis’ radiographic progression up to 26 weeks, according a new study.
While it hasn’t been formally approved yet, upadacitinib is critical to ongoing trials in treating psoriatic arthritis, Crohn’s disease, atopic dermatitis, and ulcerative colitis, alongside being considered for treating ankylosing spondylitis and giant cell arteritis. UPA was also granted breakthrough therapy designation by the US Food and Drug Administration (FDA) in 2018.
This new study’s results also further preceding evidence that upadacitinib is, in fact, consistently safe.
The SELECT-COMPARE study randomized 1629 patients to once-daily UPA 15 mg (n= 651), PBO, or ADA 40 mg (n= 327) every other week, alongside background methotrexate (MTX). From weeks 14-26, patients switched treatments if they saw less than 20% improvement in tender/swollen joint count or if the Clinical Disease Activity Index was greater than 10.
Before week 26, efficacy was judged via non-responder imputation and binary endpoints; after week 26, last observation carried forward determined continuous and binary endpoints.
Regarding patients on UPA, 38.7% were switched between weeks 14 and 16, but of those who remained on UPA, 86% completed week 48 of the study. Patients on ADA, on the other hand, saw 48.6% switched between weeks 14 and 26, and of those who remained, only 76% completed week 48. Those who did not complete the study largely exited due to actual or predicted adverse events.
Cumulative exposures were 1243.3 patient-years (PYs) for UPA and 467.8 PYs for ADA. At week 26, week 48, and additional checkpoints, UPA was significantly more effective at improving signs and symptoms based on the rheumatoid arthritis classification criteria ACR scale, and achieving clinical remissions based on Disease Activity Score 28 C-Reactive Protein.
UPA also slowed radiographic progression far more effectively than the placebo in weeks 26-48. UPA even had a lower rate of adverse events than did ADA, with the exception of Herpes zoster.
"These data continue to support the potential of upadacitinib to help maintain consistent disease control for patients living with moderately to severely active rheumatoid arthritis," said Professor Ronald van Vollenhoven, MD, PhD, Amsterdam Rheumatology and Immunology Center, Amsterdam, The Netherlands, in a statement.
These results further confirm the additional integrated safety analyses, which took place across 5 SELECT phase 3 studies.
"While remission is the primary treatment goal, in accordance with the American College of Rheumatology and the European League Against Rheumatism recommendations, a majority of patients do not achieve clinical remission today, despite currently available treatment options," van Vollenhoven said.
The study was funded by global biopharmaceutical company AbbVie, which also discovered and developed upadacitinib. Marek Honczarenko, MD, PhD, vice president of Immunology Development at AbbVie, said the study adds to the past decade of critical advances in understanding RA management—and the pursuit of achieving patient remission.
"As data continue to emerge from the SELECT program, we look forward to deepening our understanding of the benefits and risks of JAK inhibition on treatment outcomes in different patient populations with moderately to severely active rheumatoid arthritis," Honczarenko said.
The study was presented at the 2019 European Congress of Rheumatology (EULAR).




