Article
The use and misuse of injectable corticosteroids for the painful shoulder
Injectable corticosteroids may be used for managing painful shoulder conditions, but there are no universally accepted guidelines for dosage and administration. Understanding the mechanisms of action is critical for knowing when they can be used effectively. The biggest absolute contraindication to intra-articular or extra-articular corticosteroid injections is evidence or probability of infection. Relative contraindications include anticoagulation therapy, hemarthrosis, and poorly controlled diabetes mellitus. Most complications result from frequent use and can be avoided with appropriate doses and dosing intervals. Intra-articular and periarticular corticosteroid injections may cause significant systemic effects. The misuse of corticosteroid injections often is overuse. Creation of uniform guidelines for injections would help reduce their deleterious effects and maximize pain relief. (J Musculoskel Med. 2008;25:78-98)
ABSTRACT: Injectable corticosteroids may be used for managing painful shoulder conditions, but there are no universally accepted guidelines for dosage and administration. Understanding the mechanisms of action is critical for knowing when they can be used effectively. The biggest absolute contraindication to intra-articular or extra-articular corticosteroid injections is evidence or probability of infection. Relative contraindications include anticoagulation therapy, hemarthrosis, and poorly controlled diabetes mellitus. Most complications result from frequent use and can be avoided with appropriate doses and dosing intervals. Intra-articular and periarticular corticosteroid injections may cause significant systemic effects. The misuse of corticosteroid injections often is overuse. Creation of uniform guidelines for injections would help reduce their deleterious effects and maximize pain relief. (J Musculoskel Med. 2008;25:78-98)
Injectable corticosteroids, popular in the 1950s because they relieved pain in arthritic joints,1,2 are used widely now for managing a variety of painful articular and nonarticular shoulder conditions.3 When 1 or more separate but adjacent regions may be the anatomical source of shoulder pain, corticosteroids often are used in combination with local anesthetics-the anesthetic provides immediate site-specific pain relief and helps confirm injection accuracy.
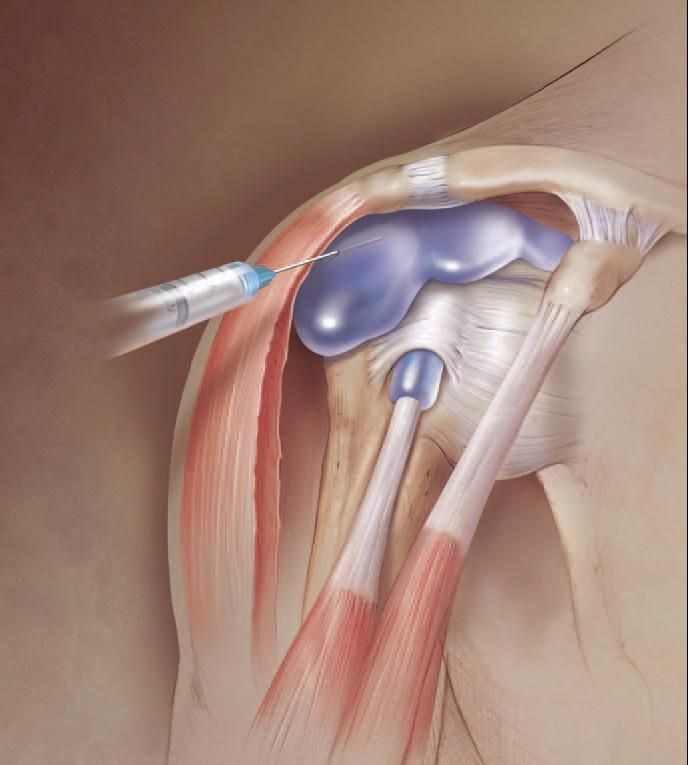
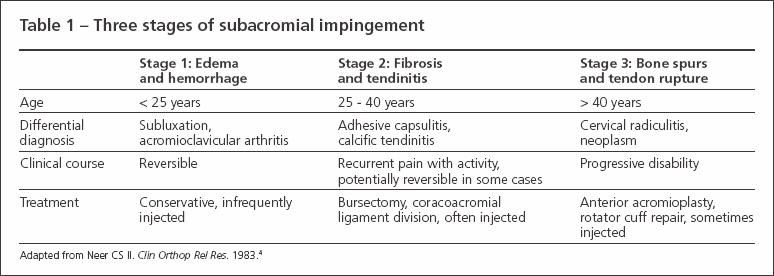
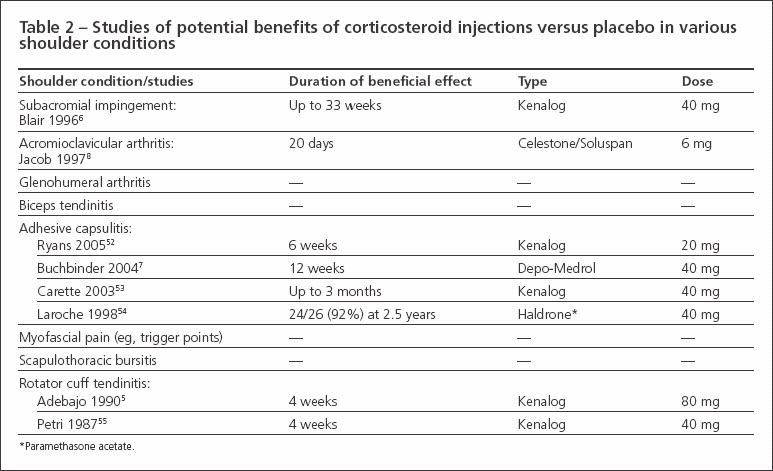
Corticosteroid/anesthetic injections are potentially curative as well as diagnostic for some subacromial (SA) impingement syndromes (Figure), such as bursitis and rotator cuff tendinitis (Table 1),4 and are beneficial in managing other painful shoulder conditions, such as osteoarthritis and adhesive capsulitis (Table 2).1,5-10 However, there are no univer
sally accepted guidelines for dosage and administration for the various shoulder conditions.11-13
Figure –
Injectable corticosteroids often are used in combination with local anesthetics for relieving shoulder pain when 1 or more separate but adjacent regions may be the anatomical source of the pain. Corticosteroid/anesthetic injections may be both curative and diagnostic for some subacromial (SA) impingement syndromes, such as bursitis and rotator cuff tendinitis. We recommend beginning with the lateral or posterolateral approach to the SA space.
In our shoulder specialty clinic, for example,we observe considerable variance in the administration and medical-record doc
umentation of corticosteroid/anesthetic injections by our referring orthopedic surgeons, primary care physicians, and other nonsurgeon health car
e professionals. There is a common lack of clarity about where the injection or injections were given (were both the SA space and acromioclavicular [AC] joint injected?) and the estimated percent relief attributed to the rapid effect of the local anesthetic. In a survey of 169 physicians (orthopedic surgeons and nonsurgeons) in our greater referral area, we found that these 2 groups often differ in the amounts of local anesthetic and corticosteroid used to inject for the same shoulder condition.12
In this 3-part article, we describe the diagnostic and therapeutic uses and misuses of corticosteroid/anesthetic injections for painful shoulder conditions. This first part reviews the mechanism of action of corticosteroids, current preparations, indications and contraindications, adverse effects, misuses, and lack of uniform standards of care. In the second part, to appear in a later issue of this journal, we will discuss the physical examination and radiographic evaluation. The third part will illustrate techniques for administering injections for specific shoulder conditions. We hope that this discussion will encourage the development of more uniform guidelines for musculoskeletal specialists and general-practice professionals, help improve injection accuracy, and enhance communication about estimation and documentation of immediate percent relief resulting from the local anesthetic.
MECHANISMS OF ACTION
Understanding the mechanisms of action of corticosteroids is critical for knowing when they can be used for treatment and why they are more potent than NSAIDs for painful shoulder conditions. The inflammatory process begins with activation of phospholipase A2, which converts phospholipids to arachidonic acid. Mediators of inflammation are then produced from arachidonic acid, which is converted into endoperoxides by cyclooxygenase (COX) or into hydroperoxides by lipoxygenase. Endoperoxides and hydroperoxides are further converted into other inflammatory mediators.
Corticosteroids are potent anti inflammatory medications that inhibit phospholipase A2, which prevents the formation of arachidonic acid, blocking synthesis along the COX and lipoxygenase pathways. They reduce prostaglandin synthesis by up to 50% and decrease interleukin-1 secretion by synovial membranes.14,15
Corticosteroids also decrease immune cell migration and reduce the vasodilatation and increased vessel permeability that accompany inflammation.3,16,17 This action increases the concentration of hyaluronic acid in arthritic joints, which is beneficial because there is an associated increase in viscosity of the synovial fluid (lower viscosity increases forces that can degenerate cartilage and reduces nutrient availability and waste removal functions that are vital for the survival of articular cartilage). These effects contribute to the potency of corticosteroids in decreasing inflammation and swelling, which reduces pain and increases joint mobility.
In contrast to corticosteroids, NSAIDs and aspirin inhibit the COX pathway. By blocking both the COX and lipoxygenase pathways, in addition to other effects, corticosteroids are superior to NSAIDs in exerting anti-inflammatory effects. In addition, injectable corticosteroids have direct access to painful joints and specific periarticular locations. However, 3 to 5 days usually are required for the corticosteroid to take full effect and all patients who receive these injections for painful shoulder conditions are informed about that.
AVAILABLE PREPARATIONS
Several injectable corticosteroids are available. Significant differences in their solubilities could correlate with differences in systemic spread and duration of local effectiveness. Our recent survey of surgeons and nonsurgeon physicians who manage painful shoulder conditions with various corticosteroid/anesthetic injections showed variations in the types used by these physician groups, including notable variations in anesthetic doses.12 Orthopedic surgeons typically use somewhat larger volumes, possibly reflecting the greater importance that surgeons place on the diagnostic aspects of the injection (eg, for surgical planning).
Fluorinated corticosteroids are more strongly associated with tendon rupture and subcutaneous atrophy than are nonfluorinated corticosteroids.18 Therefore, fluorinated corticosteroids are not recommended for use in extra-articular injections.
Our survey results suggest that orthopedic surgeons tend to be less cognizant of this issue than nonsurgeons when they select a corticosteroid type for extra-articular injections. Only 17% of surveyed rheumatologists and 8% of primary care sports medicine physicians and physical medicine and rehabilitation (PM&R) physicians typically use fluorinated corticosteroids for injecting the biceps tendon sheath, compared with 37% of orthopedists. In addition, only 10% of rheumatologists and 5% of primary care sports medicine physicians and PM&R physicians use them for injecting shoulder trigger points, compared with 34% of orthopedists.
INDICATIONS AND CONTRAINDICATIONS
Indications
Corticosteroid injections should be used only when their effects can decrease the inflammatory response. They may be beneficial in numerous extra-articular and intra-articular disorders. Shoulder diagnoses often managed with corticosteroid injections include arthritis, tendinitis, tenosynovitis, bursitis, SA impingement syndromes, and nonacute sprains and strains.1,3
Contraindications
Absolute. The biggest absolute contraindication to intra-articular or extra-articular corticosteroid injections is evidence or probability of infection.3,11 The presence of an active infection in overlying skin or tissues surrounding the shoulder joint greatly increases the risk of the injection inoculating the joint or periarticular tissues. Otherwise, the risk of inoculating the shoulder is on the order of 1:15,000, but it may be higher in patients with rheumatoid arthritis (RA).19 Other contraindications include skin breakdown or “irritation” near the proposed injection site (eg, abrasions, dermatitis, or psoriasis), poorly controlled bleeding diatheses, and hypersensitivity to corticosteroids.
Relative. These contraindications include anticoagulation therapy, hemarthrosis, poorly controlled diabetes mellitus (DM), joint instability, and limited efficacy of previous injections. Injection of painful but nonarthritic AC and glenohumeral (GH) joints in young patients or athletes might exacerbate the injury by reducing pain-related perception, which helps “protect” the joint by limiting its use.13,20
Similarly, pain relief with corticosteroid injections into degenerative joints may accelerate the degenerative process by allowing for increased use-and further deterioration-of the joint.21 However, this notion typically is based on observations in weight-bearing joints and is controversial.
ADVERSE EFFECTS
Local effects
Most complications of injectable corticosteroids result from frequent use and can be avoided with use of appropriate doses and dosing intervals. Repeated injections have been causally associated with tendon rupture, fat atrophy, dermal pigmentation, infection, and muscle wasting.1,18,20,22-24
Corticosteroid arthropathy. Deleterious consequences of intra-articular injections seen in studies of subprimate animals appear to have convinced most physicians that similar consequences might also occur in degenerative joints in humans.25 However, Balch and associates26 studied knee radiographs of 65 patients with osteoarthritis or RA who received repeated injections; the study results in most of the patients do not support the contention that repeated intra-articular injections of corticosteroids into arthritic knees would lead to rapid joint destruction.
In 1983, Gray and Gottlieb27 concluded that the concept of corticosteroid arthropathy was based largely on subprimate animal studies and several anecdotal case reports; investigations of primate (monkey) models have shown no significant long-term deleterious effect on cartilage.28 Jacoby29 studied the effects of intra-articular injections of hydrocortisone on human articular cartilage and determined that hydrocortisone does not have a catabolic effect on proteoglycan. These results, although decades old, call into question the validity of studying subprimate animal models in the context of extrapolating the possibility of inducing corticosteroid arthropathy in humans.
Rotator cuff tendon problems. Watson30 noted that a series of 4 or more preoperative SA corticosteroid injections was associated with “softer” residual rotator cuff tendons and a poorer outcome after open rotator cuff repair. However, this study did not describe the details of the injections, including the type of corticosteroid used, the dose, and the injection interval. In a retrospective review of the results of rotator cuff repairs, Bjrkenheim and coworkers31 observed that a series of more than 3 preoperative SA corticosteroid injections is associated with failure of rotator cuff repair; again, the nature and details of the injections were not described.
Histological effects. Tillander and associates32 studied the histological effects of corticosteroids using triamcinolone injections into the SA space of female rats (which resembles the human SA space) in a dosage equivalent to that given to humans. They found necrosis and collagen bundle fragmentation in the rotator cuff tendons with 5 or more repeated injections. Also using a rat model, Akpinar and colleagues33 examined the adverse effects of repeated SA injections of methylprednisolone and betamethasone, both at a dosage equivalent to that given to humans. In both of the groups, the corticosteroid-injected tendons were found to be softer and lighter in color than the tendons exposed to saline solution. Histological changes, including evidence of necrosis, collagen bundle fragmentation, and infiltration of inflammatory cells, were also present after repeated SA corticosteroid exposure. The results of these 2 studies clearly demonstrate the detrimental effects of multiple SA corticosteroid injections given at short intervals to rotator cuff tendons.
In another rat model, Wei and coworkers34 found that when an injured rotator cuff is injected, there is no deterioration in the acute phase response of the injury. When they injected the same amount onto a noninjured cuff, however, the injection initiated a short-term response similar to that seen with an acute injury. Assuming that extrapolating these data to humans is valid, the results suggest that collagen composition could be altered for 2 to 3 weeks by a single corticosteroid dose onto a grossly normal tendon, but there are no long-term effects. This finding supports waiting about 2 or 3 weeks after an SA or GH injection before the patient starts unassisted overhead lifting activities. However, we usually recommend starting a stretching and active-assisted (eg, with pulleys) lifting program 1 week after these injections.
Corticosteroid flare. Although patients typically experience significant improvement immediately after shoulder corticosteroid injections because of the local anesthetic, they should be warned that corticosteroid flare could increase their pain substantially over the preinjection level 8 to 24 hours later. Corticosteroid flare is characterized by local irritation of synovial and subcutaneous tissue, as well as pain in the general vicinity of the injection; it affects 1% to 10% of patients.1,24
The cause of corticosteroid flare is unknown, but hypotheses suggest that it represents an idiosyncratic reaction to the preservative used in injectable corticosteroid products or that it is caused by a reaction to the corticosteroid itself (eg, degradation of the corticosteroid). The low incidence of corticosteroid flare makes it unlikely that irritation of nerve endings by needle penetration is the cause. Patients who have calcific tendinitis are prone to having a substantial postinjection flare because, in theory, calcium crystals may be released from the calcific lesion, presumably intensifying the effect. The intense pain of corticosteroid flare may be managed with ice packing at the injection site and use of oral anti-inflammatory medications and analgesics, which often include narcotic medications.
Systemic effects
There is evidence suggesting that intra-articular and periarticular corticosteroid injections may cause significant systemic effects, potentially exacerbating immunosuppression by reducing the production of endogenous plasma cortisol and suppressing the hypothalamic-pituitary axis for 2 to 7 days after a single injection.20,35-37 Systemic complications of intra-articular or periarticular corticosteroid injections typically occur with high or frequent dosing or both. Flushing is seen in as many as 5% of patients.1,22
Menstrual irregularities and uterine bleeding have been reported with use of more than 40 mg of triamcinolone or the equivalent in both intramuscular and intra-articular injections.38 Studies in chickens also have shown osteonecrosis resulting from systemic corticosteroid injections,39 but no reports have clearly documented that this might be a consequence of local injections for painful shoulder conditions.24
Systemic effects are especially problematic for patients with DM or other diseases that suppress the immune system, such as RA.23,36,40,41 For example, oral corticosteroids can exacerbate glucose intolerance in patients with DM.42 One study similarly showed that long-term use of oral corticosteroids for RA may cause DM or worsen glycemic control in patients with existing DM.43 Another study concluded that overdose administration of corticosteroids can lead to a high frequency of DM.44 Although these studies of oral corticosteroid use support the general impression that blood glucose control in patients with DM also can deteriorate after intra-articular or periarticular corticosteroid injections,23,40 until recently this evidence has been little more than anecdotal.
Results of the more recent study conducted by Wang and Hutchinson41 further support the notion that hyperglycemia may be a significant postinjection problem in insulin-dependent and non–insulin-dependent patients with DM. However, the results of another recent study did not support generalizing these findings to other shoulder conditions, such as adhesive capsulitis.45
We typically receive reports of broad fluctuations in fingerstick blood glucose measurements in our insulin-dependent and non–insulin-dependent patients with DM who receive corticosteroid injections for SA impingement syndromes or adhesive capsulitis or both. We hypothesize that the one reason may be that our patients who have DM with adhesive capsulitis typically receive corticosteroid injections into both the SA space and GH joint. It may be the SA injection that is associated with the increased probability of systemic spread.
To avoid broad fluctuations in blood glucose level after shoulder corticosteroid injections, we tell our patients with DM to check their blood glucose level every 4 to 6 hours and adjust their doses as needed for 5 to 7 days postinjection. In our recent study, only 10% of 150 surveyed physicians who injected for painful shoulder conditions reported any change in methods or doses for injecting for painful shoulder conditions in their patients with DM.12 Most physicians simply injected less corticosteroid. A few avoided injecting patients with DM because of potential problems associated with poor blood glucose control. Controlled studies of various shoulder conditions are needed to establish what adjustments of corticosteroid types and doses are needed when injecting intra-articular and periarticular shoulder locations in patients with DM.
MISUSES OF INJECTIONS
Acute injuries and other considerations in athletes
In many cases, the misuse of corticosteroid injections is overuse. Clinicians’ typical avoidance of corticosteroid injections in acutely injured regions is based on clinical observations and experimental studies that suggest that corticosteroid exposure is associated with tendon and ligament atrophy, fragmentation of collagen bundles, decreased biomechanical properties, and delayed healing.13,34
Corticosteroid injections might be indicated if the symptoms have not decreased significantly after about 2 or 3 weeks of treatment with NSAIDs, analgesics, rest, and physical therapy, allowing for healing to be well under way before the injection is given. However, some surgical sports medicine specialists do not share our favorable view of corticosteroid injections for managing many shoulder conditions. The negative view is epitomized by that of Snibbe and Gambardella,13 who stated that there is no clear, objective evidence for intra-articular corticosteroid injections for managing osteoarthritic or sports-related injuries of knees, ankles, shoulders, AC joints, lumbar facet joints, and smaller hand and foot joints and that injections around joints are associated with significant risk.
However, even these investigators conceded that there may be cases in which subacute and chronic injuries also may be managed with corticosteroid injections. Examples might include post-traumatic SA impingement/bursitis in a football player who fell onto his shoulder and shoulder pain in a middle-aged women resulting from pulling weeds in her garden.
With post-traumatic bursitis, however, bleeding can occur in the vicinity of the SA bursa; therefore, a corticosteroid injection would not be appropriate. For this type of condition, we treat the patient with NSAIDs, analgesics, rest, and physical therapy for 2 or 3 weeks. If there still are significant signs of SA impingement-type pain after this period-during which the tissues have had a chance to heal-a corticosteroid injection may be considered. Failure to improve the patient’s pain with 1 postinjury injection often warrants further workup (eg, MRI to evaluate for a tear of the rotator cuff or glenoid labrum).
In contrast, injecting the AC joint for a grade 1 or 2 (mild) AC separation more acutely may be appropriate only if the patient must return to work or the athlete must return to sports activity rapidly, because a grade 1 AC separation is mainly just painful rather than unstable. We have had success with single injections in this case, probably because the corticosteroid curtails the inflammatory process and there is minimal tissue damage and need for healing.
The tendinitis vs tendinosis distinction
Usually, “-osis” conditions (involving degeneration, attrition, and necrosis) do not respond as well to NSAIDs as do “-itis” conditions (involving inflammation).Tendinoses may require corticosteroid injections for good results, but the relief might not be long lasting. Patients with long-standing shoulder pain (eg, more than 6 months) are more likely to have tendinosis; tendinitis symptoms usually are acute or subacute (less than 3 months). Patients with tendinopathy who have long-lasting relief from an injection probably had severe but reversible tendinitis or mild tendinosis with a significant inflammatory component.
If a patient has any condition best characterized by the suffix “-itis” (eg, bursitis or tendinitis), immediately giving a corticosteroid injection may be a misuse if the pain is not moderate to severe. Instead, encourage rest, ice, and NSAIDs as first-line treatment. If symptoms are not significantly improved within 1 or 2 weeks, a corticosteroid injection may be indicated.
Physical therapy considerations
Usually, physical therapy aimed at enhancing motion in addition to specific strengthening is also recommended for SA impingement syndromes. For example, in stage 3 SA impingement (where a small to medium supraspinatus tendon tear is present), enhancing the “depressor” effect on the humeral head by the inferior rotator cuff muscles may help relieve pain by reducing encroachment of the supraspinatus tendon up against the undersurface of the acromion during overhead elevation of the arm. In such cases, we recommend starting therapy 5 to 7 days after the injection is administered (for the first 2 weeks, this program includes active-assisted motion and less than 50% maximal isometric strengthening).
Physical therapy should be ordered in cases of shoulder instability to enhance all dynamic stabilizers. Corticosteroid injections are not recommended for shoulder instability, but we often inject the SA space for the “secondary” SA impingement that can result from GH instability. In addition, specialized physical therapy programs are required by scapulothoracic bursitis (often injected) and thoracic outlet syndrome (not injected).
TOWARD ACHIEVING GUIDELINES
Our review of the current English language literature has shown a lack of universally accepted guidelines for performing corticosteroid injections for shoulder conditions. Ou
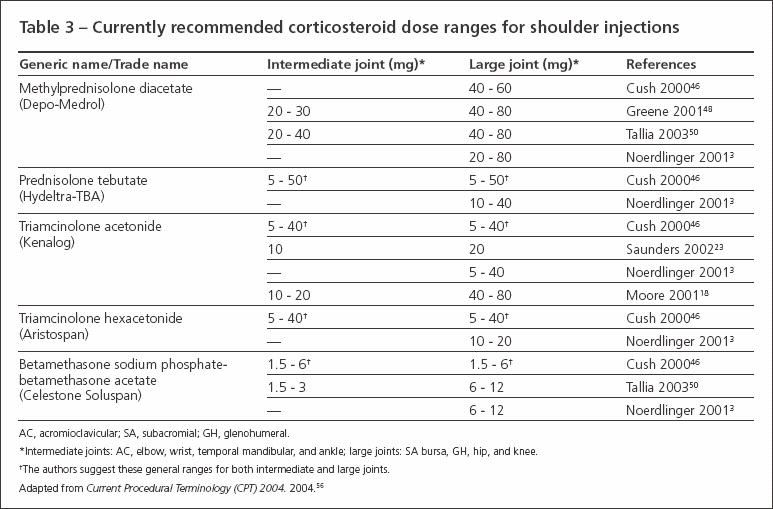
r literature review of randomized trials studying the use of corticosteroid injections for shoulder conditions also reveals a lack of consensus about dosing. Table 3 shows general recommendations for doses and dose equivalents for common injectable corticosteroids that are summarized from our clinical practice and various publications.3,20,24,35,46-51
In our recent survey, 39% of physicians reported using doses that exceed the “recommended” range for the AC joint.12 However, only a few of the surveyed physicians reported exceeding the recommended doses for the SA space and GH joint.
The creation of uniform guidelines for corticosteroid/anesthetic injections would help reduce their deleterious effects. In addition, it would help maximize pain relief for painful shoulder conditions; enhance communication between surgeons and nonsurgeons who interact in the care of patients with shoulder problems; and optimize the use of these injections for their various therapeutic, diagnostic, and prognostic purposes.
CONCLUSION
Corticosteroid injections can be a useful treatment modality for many types of painful shoulder conditions. In some cases, they might provide an alternative to surgery. If clinicians have proper knowledge and published guidelines for administering injections, they will become even more firmly established as a valuable clinical diagnostic and therapeutic tool. Part 2 of this article will focus on the physical examination for painful shoulder conditions.
References:
References
- 1. Cole BJ, Schumacher R. Injectable corticosteroid injections in modern practice. J Am Acad Orthop Surg. 2005;13:37-46.
- 2. Hollander JL, Brown EM Jr, Jessar RA, Brown CY. Hydrocortisone and cortisone injected into arthritic joints; comparative effects of and use of hydrocortisone as a local antiarthritic agent. J Am Med Assoc. 1951;147:1629-1635.
- 3. Noerdlinger MA, Fadale PD. The role of injectable corticosteroids in orthopedics. Orthopedics. 2001;24:400-405.
- 4. Neer CS II. Impingement lesions. Clin Orthop Relat Res. 1983;173:70-77.
- 5. Adebajo AO, Nash P, Hazleman BL. A prospective double blind dummy placebo controlled study comparing triamcinolone hexacetonide injection with oral diclofenac 50 mg TDS in patients with rotator cuff tendinitis. J Rheumatol. 1990;17:1207-1210.
- 6. Blair B, Rokito AS, Cuomo F, et al. Efficacy of injections of corticosteroids for subacromial impingement syndrome. J Bone Joint Surg. 1996;78A:1685-1689.
- 7. Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev. 2003;(1):CD004016.
- 8. Jacob AK, Sallay PI. Therapeutic efficacy of corticosteroid injections in the acromioclavicular joint. Biomed Sci Instrum. 1997;34:380-385.
- 9. Stefanich RJ. Intraarticular corticosteroids in treatment of osteoarthritis. Orthop Rev. 1986;15:65-71.
- 10. White RH, Paull DM, Fleming KW. Rotator cuff tendinitis: comparison of subacromial injection of a long acting corticosteroid versus oral indomethacin therapy. J Rheumatol. 1986;13:608-613.
- 11. Rozental TD, Sculco TP. Intra-articular corticosteroids: an updated overview. Am J Orthop. 2000;29:18-23.
- 12. Skedros JG, Hunt KJ, Pitts TC. Variations in corticosteroid/anesthetic injections for painful shoulder conditions: comparisons among orthopaedic surgeons, rheumatologists, and physical medicine and primary-care physicians. BMC Musculoskelet Disord. 2007;8:63-75.
- 13. Snibbe JC, Gambardella RA. Use of injections for osteoarthritis in joints and sports activity. Clin Sports Med. 2005;24:83-91.
- 14. Floman Y, Zor U. Mechanism of steroid action in inflammation: inhibition of prostaglandin synthesis and release. Prostaglandins. 1976;12:403-413.
- 15. Pelletier JP, Mineau F, Raynauld JP, et al. Intraarticular injections with methylprednisolone acetate reduce osteoarthritic lesions in parallel with chondrocyte stromelysin synthesis in experimental osteoarthritis. Arthritis Rheum. 1994;37:414-423.
- 16. Jones AK, al-Janabi MA, Solanki K, et al. In vivo leukocyte migration in arthritis. Arthritis Rheum. 1991;34:270-275.
- 17. Youssef PP, Cormack J, Evill CA, et al. Neutrophil trafficking into inflamed joints in patients with rheumatoid arthritis, and the effects of methylprednisolone. Arthritis Rheum. 1996;39:216-225.
- 18. Moore G. Arthrocentesis technique and intraarticular therapy. In: Koopman WJ, ed. Arthritis and Allied Conditions: A Textbook of Rheumatology. Philadelphia: Lippincott Williams & Wilkins; 2001:848-859.
- 19. Hollander JL. Intrasynovial corticosteroid therapy in arthritis. Md State Med J. 1970;19:62-66.
- 20. Owen D. Aspiration and injection of joints and soft tissue. In: Ruddy S, Harris ED, Sledge CB, eds. Kelley’s Textbook of Rheumatology. Philadelphia: WB Saunders Company; 2001:583-603.
- 21. Turek SL. Physiology of cartilage. In: Turek SL, ed. Orthopaedics: Principles and Their Application. Philadelphia: JB Lippincott Company; 1984:191-215.
- 22. Articular and periarticular corticosteroid injections. Drug Ther Bull. 1995;33:67-70.
- 23. Saunders S. Injection Techniques in Orthopaedic and Sports Medicine. London: WB Saunders; 2002.
- 24. Wise C. Arthrocentesis and injection of joints and soft tissues. In: Harris ED, Bud RC, Genovese MC, et al, eds. Kelley’s Textbook of Rheumatology. Philadelphia: WB Saunders; 2005:692-709.
- 25. Papacrhistou G, Anagnostou S, Katsorhis T. The effect of intraarticular hydrocortisone injection on the articular cartilage of rabbits. Acta Orthop Scand Suppl. 1997;275:132-134.
- 26. Balch HW, Gibson JM, El-Ghobarey AF, et al. Repeated corticosteroid injections into knee joints. Rheumatol Rehabil. 1977;16:137-140.
- 27. Gray RG, Gottlieb NL. Intra-articular corticosteroids: an updated assessment. Clin Orthop. 1983;177:235-263.
- 28. Gibson T, Burry HC, Poswillo D, Glass J. Effect of intra-articular corticosteroid injections on primate cartilage. Ann Rheum Dis. 1977;36:74-79.
- 29. Jacoby RK. The effect of hydrocortisone acetate on adult human articular cartilage. J Rheumatol. 1976;3:384-389.
- 30. Watson M. Major ruptures of the rotator cuff. The results of surgical repair in 89 patients. J Bone Joint Surg. 1985;67B:618-624.
- 31. Björkenheim JM, Paavolainen P, Ahovuo J, Slätis P. Surgical repair of the rotator cuff and surrounding tissues: factors influencing the results. Clin Orthop. 1988;236:148-153.
- 32. Tillander B, Franzèn LE, Karlsson MH, Norlin R. Effect of steroid injections on the rotator cuff: an experimental study in rats. J Shoulder Elbow Surg. 1999;8:271-274.
- 33. Akpinar S, Hersekli MA, Demirors H, et al. Effects of methylprednisolone and betamethasone injections on the rotator cuff: an experimental study in rats. Adv Ther. 2002;19:194-201.
- 34. Wei AS, Callaci JJ, Juknelis D, et al. The effect of corticosteroid on collagen expression in injured rotator cuff tendon. J Bone Joint Surg. 2006;88A:1331-1338.
- 35. Bird HA. Intra-articular and intralesional therapy. In: Hochberg MC, Silman AJ, Smolen JS, et al, eds. Rheumatology. Philadelphia: Elsevier; 2003:393-397.
- 36. Koehler BE, Urowitz MB, Killinger DW. The systemic effects of intra-articular corticosteroid. J Rheumatol. 1974;1:117-125.
- 37. Lazarevic MB, Skosey JL, Djordjevic-Denic G, et al. Reduction of cortisol levels after single intra-articular and intramuscular steroid injection. Am J Med. 1995;99:370-373.
- 38. Mens JM, Nico de Wolf A, Berkhout BJ, Stam HJ. Disturbance of the menstrual pattern after local injection with triamcinolone acetonide. Ann Rheum Dis. 1998;57:700.
- 39. Wang GJ, Cui Q, Balian G. The Nicolas Andry award: the pathogenesis and prevention of steroid-induced osteonecrosis. Clin Orthop Relat Res. 2000;295-310.
- 40. Black DM, Filak AT. Hyperglycemia with non-insulin-dependent diabetes following intraarticular steroid injection. J Fam Pract. 1989;28:462-463.
- 41. Wang AA, Hutchinson DT. The effect of corticosteroid injection for trigger finger on blood glucose level in diabetic patients. J Hand Surg. 2006;31A:979-981.
- 42. Nesbitt LT Jr. Minimizing complications from systemic glucocorticoid use. Dermatol Clin. 1995;13:925-939.
- 43. Panthakalam S, Bhatnagar D, Klimiuk P. The prevalence and management of hyperglycaemia in patients with rheumatoid arthritis on corticosteroid therapy. Scott Med J. 2004;49:139-141.
- 44. Xiao JZ, Ma L, Gao J, et al. Glucocorticoid-induced diabetes in severe acute respiratory syndrome: the impact of high dosage and duration of methylprednisolone therapy [in Chinese]. Zhonghua Nei Ke Za Zhi. 2004;43:179-182.
- 45. Habib GS, Abu-Ahmad R. Lack of effect of corticosteroid injection at the shoulder joint on blood glucose levels in diabetic patients. Clin Rheumatol. 2007;26:566-568.
- 46. Cush J, Kavanaugh A. Synovial fluid analysis, arthrocentesis, and joint injection techniques. In: Cush J, Kavanaugh A, eds. Rheumatology: Diagnosis and Therapeutics. Philadelphia: Lippincott Williams & Wilkins; 2000:61-73.
- 47. Genovese MC. Joint and soft-tissue injection: a useful adjuvant to systemic and local treatment. Postgrad Med. 1998;103:125-134.
- 48. Greene W. Corticosteroid injections. In: Greene W, ed. Essentials of Musculoskeletal Care. Rosemont, Ill: American Academy of Orthopaedic Surgeons; 2001:20-23.
- 49. Klippel JH, Crofford LJ, Stone JH, Weyand CM. Therapeutic injections of joints and soft tissues. In: Klippel JH, Crofford LJ, Stone JH, Weyand CM, eds. Primer on the Rheumatic Diseases. Atlanta: Arthritis Foundation; 2001:579-582.
- 50. Tallia AF, Cardone DA. Diagnostic and therapeutic injection of the shoulder region. Am Fam Physician. 2003;67:1271-1278.
- 51. Walsh NE, Rogers JN. Injection procedures. In: DeLisa JA, ed. Physical Medicine and Rehabilitation: Principles and Practice. Philadelphia: Lippincott Williams and Wilkins; 2005:311-360.
- 52. Ryans I, Montgomery A, Galway R, et al. A randomized controlled trial of intra-articular triamcinolone and/or physiotherapy in shoulder capsulitis. Rheumatology (Oxford). 2005;44:529-535.
- 53. Carette S, Moffet H, Tardif J, et al. Intra-articular corticosteroids, supervised physiotherapy, or a combination of the two in the treatment of adhesive capsulitis of the shoulder: a placebo-controlled trial. Arthritis Rheum. 2003;48:829-838.
- 54. Laroche M, Ighilahriz O, Moulinier L, et al. Adhesive capsulitis of the shoulder: an open study of 40 cases treated by joint distention during arthrography followed by an intraarticular corticosteroid injection and immediate physical therapy. Rev Rhum Engl Ed. 1998;65:313-319.
- 55. Petri M, Dobrow R, Neiman R, et al. Randomised double blind, placebo controlled study of the treatment of the painful shoulder. Arthritis Rheum. 1987;30:1040â1045.
- 56.Current Procedural Terminology (CPT) 2004. Chicago: AMA Press; 2004.




